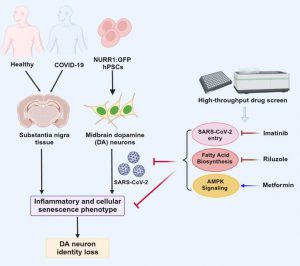
In a new study, researchers from the Will Cornell Medical Center, Memorial Sloan Kettering Cancer Center, and Columbia University’s Wagros School of Internal and External Medicine pointed out that the coronavirus SARS-CoV-2, which causes COVID-19, can infect dopaminergic neurons in the brain and cause aging, meaning they lose their ability to grow and divide. They believe that further research on this discovery may reveal neurological symptoms related to long-term COVID-19, such as brain fog, sleepiness, and depression. The relevant research results were published in the Cell Stem Cell journal, with the title “SARS-CoV-2 infection causes dopaminergic neuron senescence”.
These research results indicate that dopamine neurons infected with SARS-CoV-2 stop working and emit chemical signals that lead to inflammation. Under normal circumstances, these neurons produce dopamine, which is a neurotransmitter that plays a role in pleasure, motivation, memory, sleep, and movement. The damage to these neurons is also related to Parkinson’s disease.
Dr. Shuibing Chen, co-author of the paper and director of the Genomic Health Center at Will Cornell Medical Center, said, “The initial purpose of this project was to study how various types of cells in different organs respond to SARS-CoV-2 infection. We tested lung cells, heart cells, and pancreas β cells, but the aging pathway is only activated in dopaminergic neurons. This is a completely unexpected result. ”
Before this, Dr. Chen led research on using human stem cells to generate multiple cell types and tested them to determine which cells SARS-CoV-2 can infect. This allows them to study the tissue range that this virus may infect during COVID-19, as the symptoms of different patients are diverse. They also studied autopsy samples from patients infected with SARS-CoV-2 to confirm observations from laboratory cultured cells.
Surprisingly, they found that the proportion of infected dopaminergic neurons exposed to SARS-CoV-2 was very small, about 5%. Dr. Chen said, “The infection rate of dopaminergic neurons is not as high as that of lung cells, which are the main targets of this virus. However, even a small fraction of infected dopaminergic neurons may have serious effects.”
Interestingly, not all types of neuronal cells are susceptible to viral infections. These authors observed that under the same experimental conditions, cortical neurons did not allow SARS-CoV-2 infection.
In this paper, these authors utilized transcriptome technology to determine how SARS-CoV-2 infection alters gene activity and the resulting changes in cellular behavior. Dr. Chen said, “We found that only the aging pathway of dopaminergic neurons was activated. In contrast, the aging pathway genes in lung-like organs, pancreatic cells, liver-like organs, or heart cells infected with SARS-CoV-2 were not significantly activated.”
These authors found that the genetic characteristics – unique patterns of gene activity – of infected dopaminergic neurons cultured in the laboratory and dopaminergic neurons from autopsy samples of COVID-19 patients are the same, including genes that trigger inflammatory chemical signals.
Next, these authors seek ways to protect these neurons to reduce the risk of neurological defects in patients infected with the virus. They tested drugs available on the market to treat various diseases and found a drug that could prevent SARS-CoV-2 infection or protect infected dopaminergic neurons from aging. Their screening results showed that three drugs can prevent SARS CoV-2 infection, thus preventing dopamine cell aging: riluzole (for atrophic lateral sclerosis), metformin (for diabetes), and imatinib (for cancer). Further research on these drugs may find ways to prevent the virus from attacking the brain.
Although most people are infected with SARS-CoV-2, only some are affected because the risk of neurological symptoms is related to many factors, including the severity of the disease and genetics. Human population research is further exploring this issue.
Although the clinical significance of these findings is still unclear, because the aging of dopaminergic neurons is one of the characteristics of Parkinson’s disease, these authors suggest that the risk of Parkinson’s disease-related symptoms in patients with COVID-19 should be monitored. So far, the symptoms of Parkinson’s disease have not been extensively reported in population studies.
Reference
Liuliu Yang et al. SARS-CoV-2 infection causes dopaminergic neuron senescence. Cell Stem Cell, 2024, doi:10.1016/j.stem.2023.12.012.