Metabolic Diseases Targets
Target Search
Background
What are Metabolic Diseases?
Metabolic diseases are a kind of disease caused by the problem of metabolic process, which includes two kinds of metabolic disorders and metabolic exuberance. Metabolism refers to the chemical reactions carried out in the body to maintain life, including the production of energy, the synthesis and decomposition of substances. Metabolic diseases are often related to genetics, enzyme defects, hormonal imbalances, or lifestyle factors.
Specifically, metabolic disease symptoms may be related to the accumulation or deficiency of metabolic substances such as sugars, fats, proteins, purines, calcium and copper in the body, leading to a series of diseases, such as diabetes, hypoglycemia, gout, scurvy, vitamin D deficiency, protein-energy malnutrition, metabolic bone disease, etc. These diseases usually appear in the process of growth and development, and are accompanied by the accumulation or deficiency of a variety of metabolites, and then produce corresponding clinical symptoms.
The prevention and control of metabolic diseases, which have a significant impact on patients' quality of life, ability to work, and social economy, is therefore critical to public health. With the development of molecular biology and genetics, the understanding of metabolic diseases continues to deepen, and new therapeutic approaches and strategies are constantly being developed.
The diagnosis of metabolic diseases usually requires a combination of clinical symptoms, biochemical tests (levels of metabolites in the blood and urine), and genetic testing. Many countries implement neonatal screening programs for the early detection and treatment of certain inherited metabolic disorders such as phenylketonuria (PKU) and galactosemia.
Causes of Metabolic Diseases
Metabolic diseases are often related to genetics, enzyme defects, hormonal imbalances, or lifestyle factors. Many metabolic diseases are caused by genetic factors, and these diseases are called inherited metabolic diseases. They may result in the deficiency or abnormal function of specific enzymes due to genetic mutations, which in turn affect metabolic pathways. Factors including a high-fat, high-carbohydrate diet, as well as low labor intensity and physical activity, can increase the occurrence of insulin resistance and promote the development of metabolic syndrome. Unhealthy lifestyles such as poor eating habits, lack of exercise, smoking and drinking alcohol can all increase the risk of metabolic diseases.
Some genetic factors make patients more susceptible to certain adverse external factors than normal people. For example, people with certain types of human leukocyte associated antigens are prone to insulin-dependent diabetes, viral infections and other external factors can invade the islet cells of these susceptible individuals, resulting in autoimmune reactions and the destruction of beta cells. Sometimes, two genetic diseases can cause the same metabolic disorder, and when these two genetic diseases exist at the same time, the metabolic diseases caused by a single genetic disease is much more serious.
The pathological changes and dysfunction of internal organs are also important causes of metabolic diseases. For example, renal failure can cause metabolic changes in proteins, fats, water and electrolytes. In renal failure, blood phosphorus increases, blood calcium decreases, 25-hydroxyvitamin D cannot be hydroxylated to 1, 25-dihydroxyvitamin D in the kidney, secondary secretion of parathyroid hormone increases and acidosis, resulting in calcium and phosphorus metabolism disorders and metabolic bone diseases.
Some external factors such as drugs and food can also cause various metabolic diseases. Antiepileptic drugs such as barbiturate sodium, phenytoin sodium can promote the activity of liver microsomal enzyme, accelerate the decomposition of vitamin D and 25-hydroxyvitamin D in the liver, therefore, after long-term use of such drugs, blood 25-hydroxyvitamin D decreased, followed by blood calcium, phosphorus decreased, alkaline phosphatase increased, osteomalacia. People who regularly eat foods containing too much fat and cholesterol are prone to hyperlipoproteinemia, arteriosclerosis and cholelithiasis.
Metabolic Diseases Examples
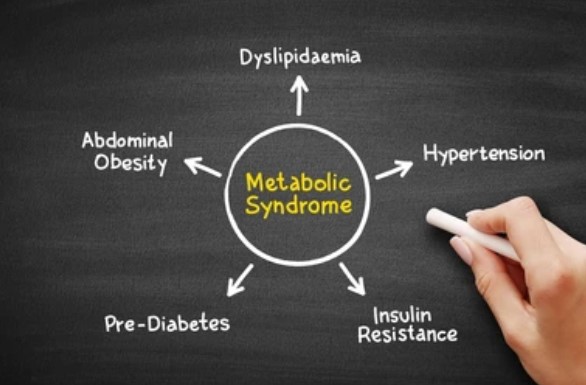
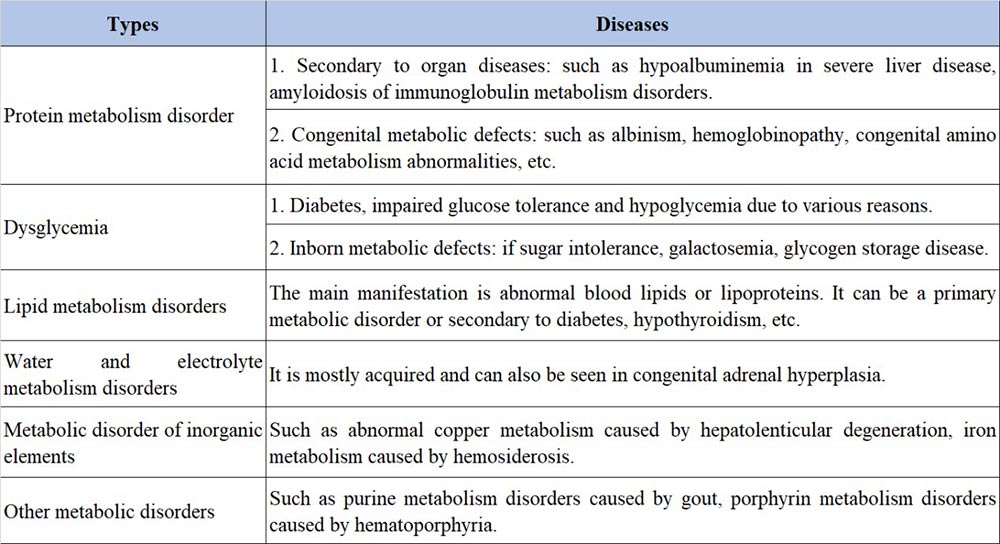
Metabolic diseases are generally classified according to the main pathways of intermediate metabolism, including protein metabolism disorders, sugar metabolism disorders, lipid metabolism disorders, water and electrolyte metabolism disorders, inorganic element metabolism disorders, and other metabolic disorders.
Symptoms of Metabolic Diseases
The symptoms of metabolic diseases are varied and often manifest as systemic dysfunction, These include, but are not limited to, fatigue and weakness, abnormal weight gain or loss, growth and development problems, skin lesions, digestive system abnormalities, muscle and joint pain, bone problems, paresthesia, cardiovascular symptoms, respiratory problems, mental health problems, endocrine disorders, and specific symptoms caused by the accumulation of certain metabolic substances. These diseases have some common characteristics, such as:

- Sugar, protein, fat and water, minerals and other metabolic disorders, often affect and link with each other, sometimes causing a vicious cycle. For example, lack of insulin increases blood sugar, increase of plasma lipoprotein, cholesterol and triglyceride, protein decomposition, negative nitrogen balance, osmotic diuresis of sugar causes dehydration and negative balance of potassium, sodium, calcium, phosphorus and magnesium, etc. In severe cases, ketoacidosis occurs, which aggravates the rise of blood sugar and blood lipids, and so on until the patient dies.
- Various metabolic diseases can affect tissues and organs throughout the body. For example, the basic feature of hypercholesterolemia is the deposition of cholesterol in blood vessels and other places, resulting in arteriosclerosis. The affected tissues are systemic, such as cerebral arteriosclerosis, coronary heart disease, renal arteriosclerosis and resulting in renal dysfunction, peripheral arteriosclerosis, and xanoma of skin and tendon.
- The severity of clinical manifestations of metabolic diseases depends on the degree of metabolic disorders and the degree of damage to the structure and function of vital organs. Generally speaking, the early stage of the disease is only the change of biochemical process, the pathological and functional changes of organ tissues are not obvious, and there are no obvious symptoms clinically. Many metabolic diseases can affect intelligence, growth and mental state. Such as phenylketonuria, cysteinuria and so on are accompanied by serious brain damage and mental decline, growth and development block, children often die early.
Treatment of Metabolic Diseases
Most metabolic diseases lack a cure. Treatment options include: alternative therapies (such as injecting insulin into insulin-dependent diabetics to supplement the lack of insulin secreted by islet beta cells); Reducing substrate accumulation due to enzyme defects (e.g. treating hemilactoidemia with foods without hemilactoidemia); Sodium bicarbonate can be used to correct the hypokalemia and hyperchloric acidosis caused by renal tubule acidosis and supplement potassium salt. D-penicillin can be combined with cystine to form a disulfide mixture that is more soluble, so it can be used to treat cystinuria.

However, daily habits also need to be adjusted. By adjusting the diet structure, controlling the total calorie intake, reducing the intake of fat and simple carbohydrates, and increasing the dietary fiber, it helps to control the weight and improve the metabolic status. Proper physical activity and physical activity can increase the body's sensitivity to insulin and improve blood lipid and blood sugar levels. For metabolic diseases caused by specific environmental factors or foods, avoiding exposure to these factors or foods is an important therapeutic measure.
Treatment from the root causes is also being further explored. Although still in the research phase, gene therapy holds promise as a treatment for certain inherited metabolic diseases. In some cases, such as type 1 diabetes or hepatolenticular degeneration, cell or organ transplants may be a treatment option. But the most important thing is to strengthen the awareness of disease prevention and patient health awareness. Regular monitoring of blood sugar, blood lipids, blood pressure and other indicators to evaluate the treatment effect and adjust the treatment plan. Patient education and self-management are also essential for long-term management of metabolic diseases.
Case Study
Case Study 1: Active Recombinant Human HMGCR protein (HMGCR-263H)
AMP-activated protein kinase (AMPK) is a metabolic sensor that maintains energy homeostasis. AMPK functions as a tumor suppressor in different cancers; however, its role in regulating antitumor immunity, particularly the function of regulatory T cells (Tregs), is poorly defined. AMPKα1fl/flFoxp3YFP-Cre, Foxp3YFP-Cre, Rag1-/-, and C57BL/6 J mice were used for our research. Flow cytometry and cell sorting, western blotting, immuno-precipitation, immuno-fluorescence, glycolysis assay, and qRT-PCR were used to investigate the role of AMPK in suppressing programmed cell death 1 (PD-1) expression and for mechanistic investigation. The results showed that metabolically, loss of AMPK in Tregs promotes glycolysis and the expression of 3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR), a key enzyme of the mevalonate pathway. Mechanistically, AMPK activates the p38 mitogen-activated protein kinase (MAPK) that phosphorylates glycogen synthase kinase-3β (GSK-3β), inhibiting the expression of PD-1 in Tregs.
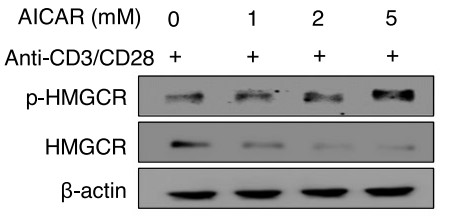
Fig1. Detection of the phosphorylated and dephosphorylated form of HMGCR from WT Tregs. (Ram Hari Pokhrel, 2021)
Case Study 2: Active Recombinant Human Insulin (Insulin -53H)
The scarcity of postmortem pancreas tissue suitable for islet cell isolation limits the use of cell replacement therapy in diabetes patients. To address this, researchers have been looking into the role of transcription factors like PDX1, PAX4, and neurogenin-3, which are known to support the development of insulin-producing beta cells. In this study, the researchers examined how PAX4 and PDX1 can influence the transformation of mesenchymal stem cells (MSCs) into insulin-secreting beta-like cells in the lab. They used specially engineered viruses to deliver PDX1 alone or in combination with PAX4 to the MSCs. Then RT-PCR, Western blot, and immunofluorescence to measure the expression of key genes and proteins, and an enzyme-linked immunosorbent assay (ELISA) were utilized to quantify insulin and C-peptide output from the treated cells in response to elevated glucose levels. The results indicate that PAX4 significantly boosts the ability of PDX1-expressing MSCs to develop into organized, functional islet-like structures that produce insulin. These findings pave the way for developing a new method to produce insulin-secreting cells from MSCs using PAX4 and PDX1, which could have significant implications for future clinical treatments.
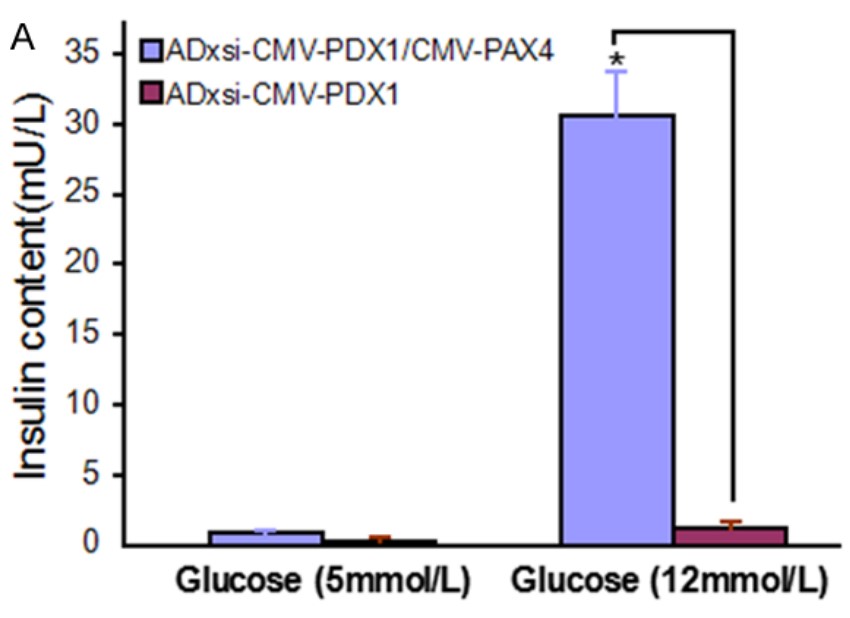
Fig2. Insulin in response to Adxsi-CMV-PDX1 or Adxsi-CMV-PDX1/CMV-PAX4. (Lifa Xu, 2017)
Case Study 3: Recombinant Human PPARG(209-477 aa) (PPARG-2772H)
The process of cutting up a specific part of a protein called L1, which is found in mouse brain cells, can be started by certain signals that the L1 protein responds to. This leads to the creation of a piece of the L1 protein that can move into the nucleus of the cell. The researchers found that there are specific patterns of amino acids, called LXXLL and FXXLF, in this L1 piece that allow it to connect with other proteins inside the cell's nucleus, like ERα, ERβ, PPARγ, and RXRβ. If these patterns are changed or damaged, the L1 piece can't connect properly with these other proteins. They also discovered that when change these patterns in mouse embryos while they're still developing in their mother, the mice grow up with problems with their movement, learning, memory, and the way their brain cells connect with each other in a part of the brain called the cerebellum. These problems are similar to those seen in mice that don't have the L1 protein at all. This tells us that the L1 protein and its interactions with other proteins in the cell's nucleus might play a big role in how brain cells connect and change over time.
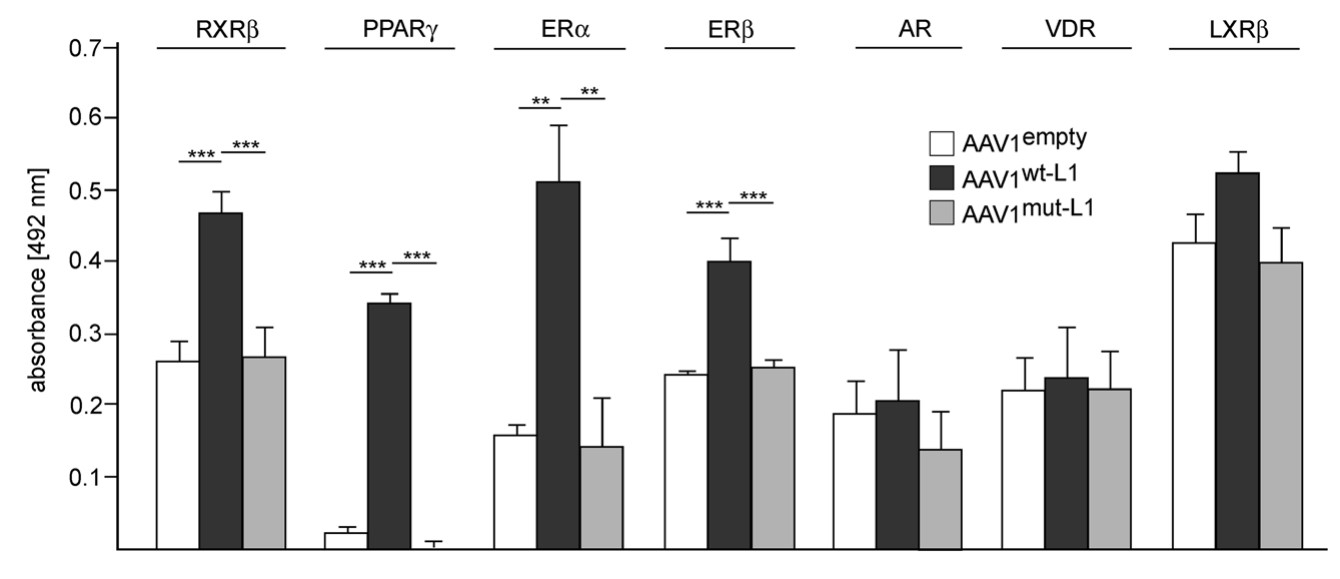
Fig3. Nuclear L1 interacts with nuclear receptors. (Kristina Kraus, 2018)
Related Resources
Metabolic diseases are disorders caused by the disruption of normal metabolic processes in the body. Metabolism refers to the chemical processes that occur within a living organism to maintain life, including the breakdown of substances for energy and the synthesis of compounds needed for cellular function. When these processes become imbalanced or dysfunctional, it can lead to various health problems known as metabolic diseases. The prevention and control of metabolic diseases, which have a significant impact on patients' quality of life, ability to work, and social economy, is therefore critical to public health. Improving the public's awareness of metabolic diseases and strengthening patient education are of great significance for improving patients' self-management ability and improving treatment effect.
Contact us or send an email at for project quotations and more detailed information.
Quick Links
-

Papers’ PMID to Obtain Coupon
Submit Now -

Refer Friends & New Lab Start-up Promotions

