Immune Diseases Targets
Target Search
Background
What are Immune Diseases?
Immune diseases, also known as immunological disorders, are a class of diseases caused by abnormal immune system function. The immune system is an important defense system of the human body, which is composed of immune organs, immune cells and immune molecules. It is responsible for identifying and removing non-self components in the body, such as pathogens such as bacteria and viruses, as well as damaged or dead cells. However, when the immune system functions abnormally, it can lead to immune diseases.
Immune diseases can be classified from different perspectives. According to the immune function, it is often divided into three diseases: immune deficiency, immune increase and allergic reaction. According to the occurrence time, it can be divided into congenital and acquired (acquired); According to the speed of development, it can be divided into fast type and delayed type. According to immune mechanism, it can be divided into cellular immunity and humoral immunity. According to the scope of disease damage can be divided into limited office, systemic (systemic); According to the nature of antigen can be divided into exogenous, allogenic, autogenic.
Treatment of immune diseases usually needs to be specific to the type and cause of the disease and may include medication, immunomodulatory therapy, avoidance of exposure to allergens, and other measures. In addition, maintaining a healthy lifestyle, a reasonable diet and a good mental state also have a positive effect on improving immunity and preventing immune diseases.

Immune Diseases List
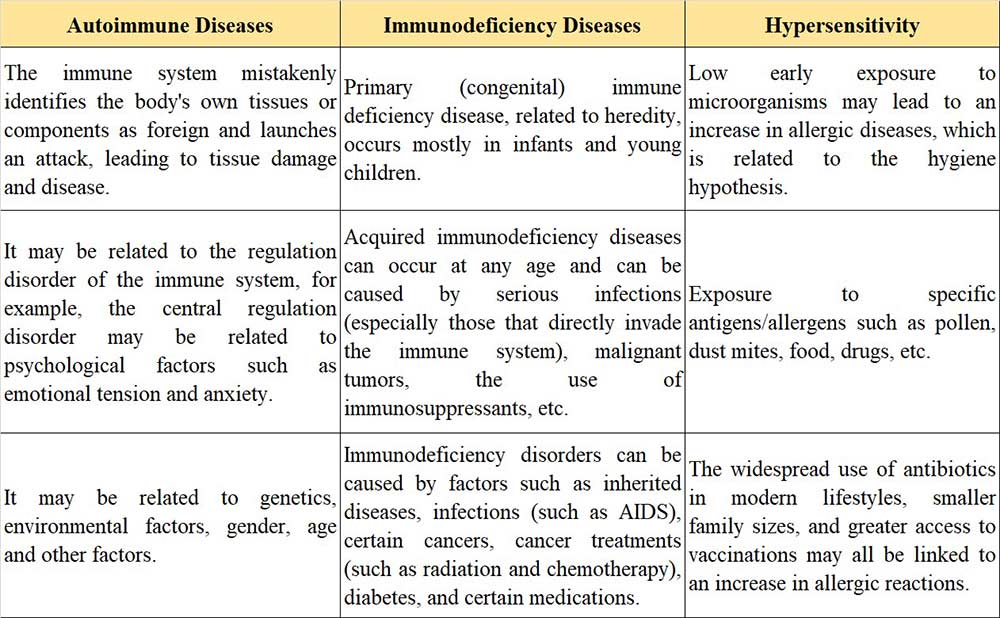
In general, immune diseases can be roughly divided into three categories, namely: The body produces an immune response against itself (autoimmune diseases). The body cannot mount an appropriate immune response to the invading microbe (immunodeficiency diseases). The body overreacts to often harmless foreign antigens and damages normal tissues (hypersensitivity).
- Autoimmune diseases occur when the immune system mistakenly recognizes the body's own tissues or components as foreign and launches an attack, resulting in tissue damage and disease. For example, systemic lupus erythematosus, rheumatoid arthritis, etc. Such diseases may be related to genetic factors, environmental factors, gender, age and other factors.
- Immunodeficiency is a condition in which one or more components of the immune system are impaired or missing, resulting in a reduced defense against pathogens. For example, acquired immune deficiency syndrome (AIDS) due to HIV infection.
- Hypersensitivity, or allergy, is an abnormal and excessive immune response of the immune system to originally harmless antigens (such as certain foods, pollen, etc.), resulting in damage to body tissues and cells.

What Causes Immune Diseases?
The pathogenic factors of immune diseases are various, and the pathogenic factors are summarized according to the classification of diseases.
Symptoms of Immune Diseases
Although there are only three broad classifications of immune diseases, there are different disease phenotypes in the specific characterization, and they are subdivided into multiple disease types. Includes: Autoimmune diseases, Immune disorders, Transplant rejection, Rheumatoid arthritis, Multiple sclerosis, Systemic lupus erythematosus, Inflammatory bowel disease, angioedema, mastocytosis and various allergic reactions.
Autoimmune Diseases: The symptoms of autoimmune diseases depend on the disease and the body organs involved. Some autoimmune diseases affect certain types of tissue throughout the body - for example, blood vessels, cartilage or skin. Other autoimmune diseases affect specific organs. Virtually any organ, including the kidneys, lungs, heart and brain, can be affected. The resulting inflammation and tissue damage can lead to pain, joint deformities, weakness, jaundice, itching, difficulty breathing, fluid accumulation (edema), delirium, and even death.
Transplant Rejection: Even if the tissue is a close match, organ transplants, unlike blood transfusions, often result in rejection if measures are not taken to prevent rejection. Rejection results from the recipient's immune system attacking the transplanted organ, which is recognized by the immune system as a foreign body. Rejection can be mild and easily controlled, or it can be severe and still worsen treatment. In severe cases, complications such as infection, cancer, atherosclerosis, and kidney problems can occur.
Rheumatoid arthritis: Rheumatoid arthritis is a chronic inflammatory disease that primarily affects the joints, but may also affect other body systems. The most obvious are joint pain, joint stiffness, joint swelling, and joint deformity. There may also be fever, fatigue and weakness, loss of appetite, weight loss, night sweats of hands and legs, general discomfort, etc., or anemia, lung disease, cardiovascular disease, depression, superficial lymph node enlargement, liver and kidney damage.
Multiple sclerosis: In multiple sclerosis, an inflammatory response by the immune system leads to damage to the myelin sheath and is a chronic disease that affects the central nervous system. Accompanied by limb weakness or numbness, tingling, numbness or burning, ataxia, muscle stiffness and spasms. Other symptoms include memory problems, cognitive impairment, mood instability or depression, problems with sexual function, bowel and bladder function and vision problems.
Systemic lupus erythematosus: Systemic lupus erythematosus is a systemic autoimmune disease with a variety of symptoms, most common in young women, It can affect the skin (e.g., butterfly erythema, light sensitivity), joints (causing joint pain and swelling), kidneys (nephritis or nephrotic syndrome), heart (pericarditis, myocarditis), lungs (pleuritis, pneumonia), blood system (anemia, leukopenia), nervous system (headaches, seizures, psychiatric symptoms), and digestive system (nausea, vomiting, abdominal pain) System.
Inflammatory bowel disease: Inflammatory Bowel Disease (IBD) is a group of chronic inflammatory diseases that primarily affect the gastrointestinal tract, especially the colon and ileum. Symptoms are characterized by abdominal pain, diarrhoea, bloody stools, weight loss, appetite loss, fatigue, and malnutrition. Specific conditions can present as inflammation and ulceration of the entire intestinal wall in Crohn's disease, and inflammation and ulceration of the colon mucosa in Ulcerative colitis.
Angioedema: Angioedema is a transient, localized edema of the skin and submucosal tissues characterized by sudden, painless, non-inflammatory swelling of the skin that is common in the face, extremities, and genital areas and may be accompanied by difficulty breathing, gastrointestinal symptoms (such as abdominal pain, nausea), and low blood pressure.
Mastocytosis: Mastocytosis is a rare disease involving abnormal proliferation of mast cells in the skin and/or other organs, with symptoms including red spots on the skin, itching, hives, swelling of the skin, and possibly systemic symptoms such as abdominal pain, nausea, vomiting, diarrhea, headache, palpitations, low blood pressure and bone pain. These symptoms may be due to systemic reactions to mediators released by mast cells, such as histamine.
Other allergic reactions: An allergic reaction is an abnormal immune response to a foreign substance (allergen) that is normally harmless. It is characterized by skin symptoms (e.g., hives, eczema), respiratory symptoms (e.g., nasal congestion, asthma), digestive symptoms (e.g., nausea, diarrhea), cardiovascular symptoms (e.g., hypotension, palpitations), and in severe cases, anaphylactic shock. These symptoms can occur quickly after exposure to an allergen and require prompt identification and treatment to avoid potentially life-threatening conditions.

Immune Diseases Treatments
The prevention and treatment of immune diseases can follow the following principles:
- Alternative therapy or immune booster can be used for immune deficiency;
- Remove or avoid allergenic substances to prevent immune responses;
- Specific desensitization therapy can be used for type I allergy to improve the body's tolerance to allergenic antigens;
- Type I allergy can also use mast cell stabilizer, such as sodium chromoglycate to prevent mast cell reaction;
- Use drugs to resist mediators released during allergy (such as antihistamines to antagonize the effect of histamines) or relieve tissue reactions caused by these mediators (such as vasoconstrictors to treat anaphylactic shock), and use bronchodilators to treat bronchial asthma;
- Use immunosuppressants to suppress overactive immune responses, such as severe immune complex diseases, autoimmune diseases, and immunoproliferative diseases;
- To remove infectious foci that stimulate immune response and foci that produce autoantigens;
- The elimination of various stimuli that can aggravate the clinical symptoms of immune diseases, such as dust, environmental pollution, fatigue, mental stimulation, nasal polyps that hinder nasal breathing, curved nasal septum, and enlarged tonsils and adenoids that hinder breathing.

In addition, immunotherapy is evolving rapidly, and several types (classes) of immunotherapy drugs have been developed. Some of the most common categories are: cytokines and cytokine receptors, fusion proteins, and monoclonal antibodies.
Cytokines are chemical messengers of the immune system. White blood cells and certain other cells of the immune system produce cytokines when they detect foreign bodies (antigens). Examples of cytokines include interferon and interleukin. Cytokines transmit their messages by attaching to specific molecules called receptors on the surface of another cell. Cytokines and their receptors are kind of like keys and locks. Different cytokines have different receptors. Cytokines or their receptors can be produced in the laboratory. When given to humans, artificial cytokines, or cytokine receptors, can be used to alter the body's natural immune response and treat many diseases.
Fusion proteins are compounds created in the laboratory that combine, or "fuse" together, two different proteins with desirable immune modification and disease-fighting properties to form a drug. When given to humans, the newly produced fusion proteins can be used to modify the natural immune response and treat a wide range of diseases. An example of a fusion protein is the drug Etanercept, which causes cytokine receptors to fuse with antibodies.
Monoclonal antibodies (Mabs) are antibodies produced in the laboratory from living cells that have been altered to produce the desired antibody. When injected into the human bloodstream, they act like antibodies produced by the body. Monoclonal antibodies are often designed to attack cancer cells or substances that cause inflammation in diseases such as rheumatoid arthritis.
Case Study
Case Study 1: Recombinant Human AHCY (AHCY-31342TH)
DNA methylation plays a crucial role in the growth and functioning of mammals. In this study, the researchers discovered that the H19 long non-coding RNA (lncRNA), which changes during development, interacts with and suppresses the activity of S-adenosylhomocysteine hydrolase (SAHH). In vitro rSAHH activity assays were designed to test whether binding of H19 RNA fragments to rSAHH would inhibit rSAHH enzymatic activity in vitro. The findings indicate that when the H19 lncRNA is reduced (knocked down), it activates SAHH, resulting in heightened methylation activity by DNMT3B, a key enzyme involved in DNA methylation. This leads to increased methylation of the Nctc1 gene, which is controlled by an lncRNA. Comprehensive analysis of DNA methylation across the genome has unveiled alterations at many gene loci that align with the influence of H19 on SAHH. The results proposed a surprising regulatory mechanism involving widespread epigenetic changes instigated by a single, highly expressed lncRNA.
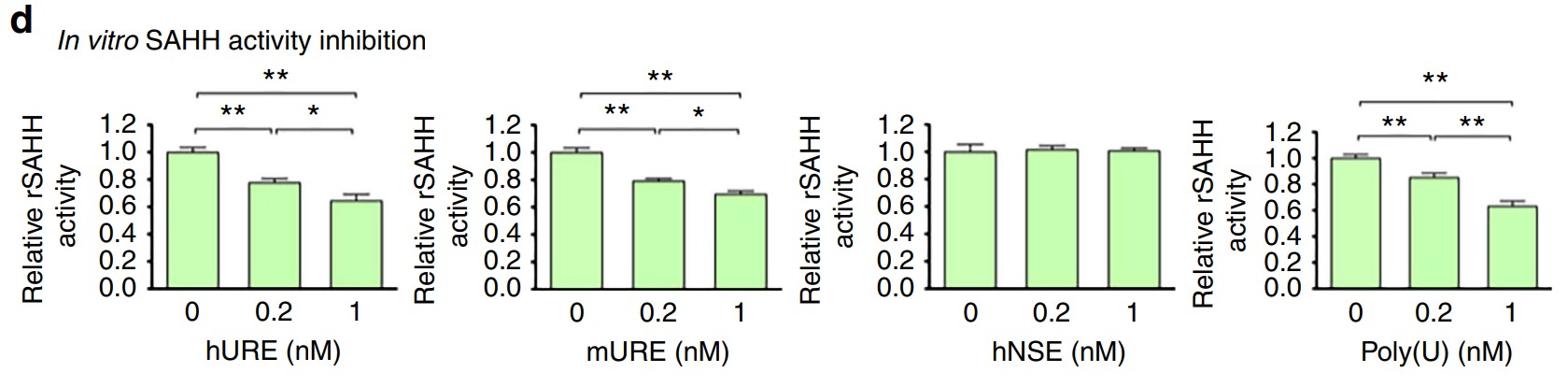
Fig1. In vitro rSAHH activity assay. (Jichun Zhou, 2015)
Case Study 2: Recombinant Human TNF protein (TNF-412H)
This study aims to evaluate the effects that early and late systemic administration of methylprednisolone have on lungs in a rat model of brain death. Twenty-four male Wistar rats were anesthetized and randomly divided into four groups. All of the animals were observed and ventilated for 120 min. And they determined hemodynamic and arterial blood gas variables; wet/dry weight ratio; histological score; levels of thiobarbituric acid reactive substances (TBARS); superoxide dismutase (SOD) activity; and catalase activity. Myeloperoxidase activity, lipid peroxidation, and TNF-α levels were assessed in lung tissue. In this model of brain death, the early and late administration of methylprednisolone had similar effects on inflammatory activity and lipid peroxidation in lung tissue.
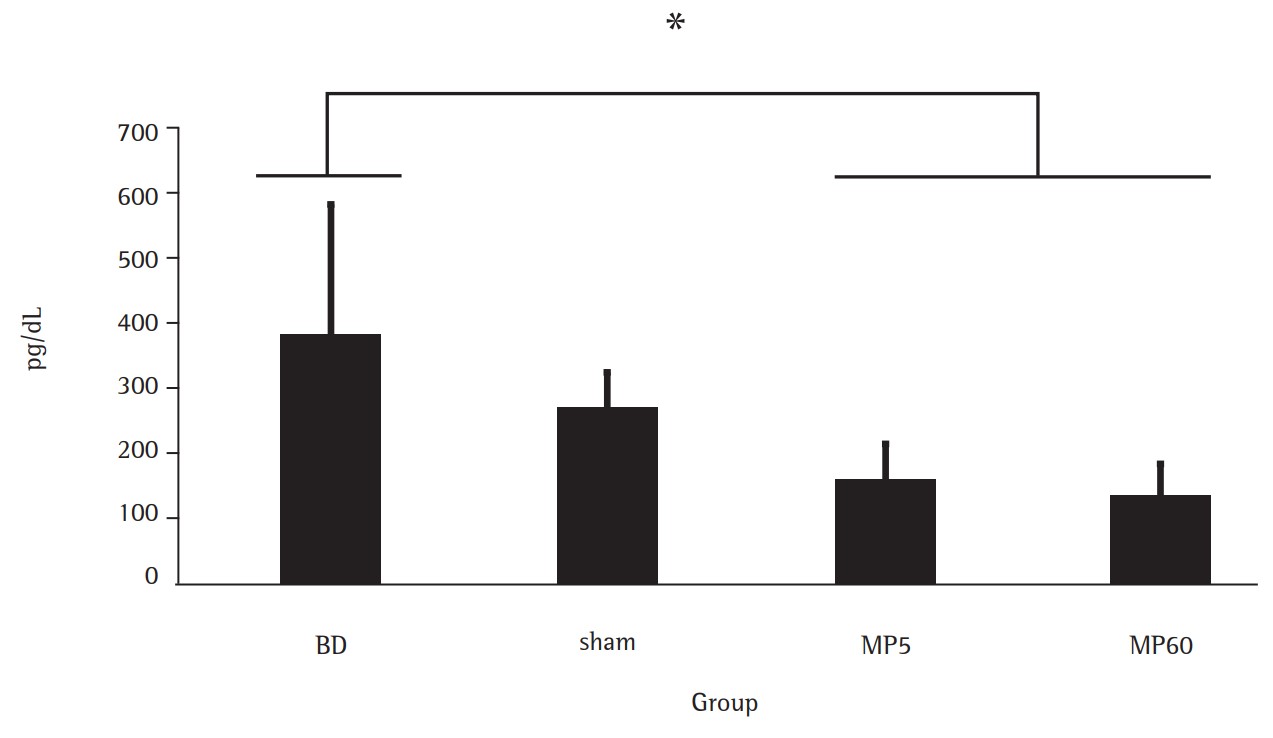
Fig2. TNF-α levels in lung tissue. (Eduardo Sperb Pilla, 2013)
Case Study 3: Recombinant Human CXCR4 (CXCR4-504H)
Previous studies have shown that topical stromal cell-derived growth factor-1 (SDF1) promotes neovascularization in diabetic mice, leading to faster re-epithelialization of skin wounds. However, the clinical use of this bioactive peptide is limited because they degrade rapidly in the wound environment due to high levels of proteases. Here, the ability of recombinant fusion proteins composed of SDF1 and elastin like peptides to self-assemble into nanoparticles was investigated. By measuring the equilibrium dissociation constant (Kd) of binding of free SDF1 or fusion protein to CXCR4 receptor, it can be seen that fusion protein and recombinant human SDF1 have similar binding properties. The biological activity of SDF1-ELP is very similar to that of free SDF1. In contrast, the bioactivity of SDF1-ELP in vivo is significantly superior to that of free SDF1. When SDF1-ELP nanoparticles were applied to full-layer skin wounds of diabetic mice, the wound healing ability was better than that of free SDF1, ELP alone or drug-loaded treatment. At the same time, SDF1-ELP nanoparticles significantly increased the epidermis and dermis of healed wounds.
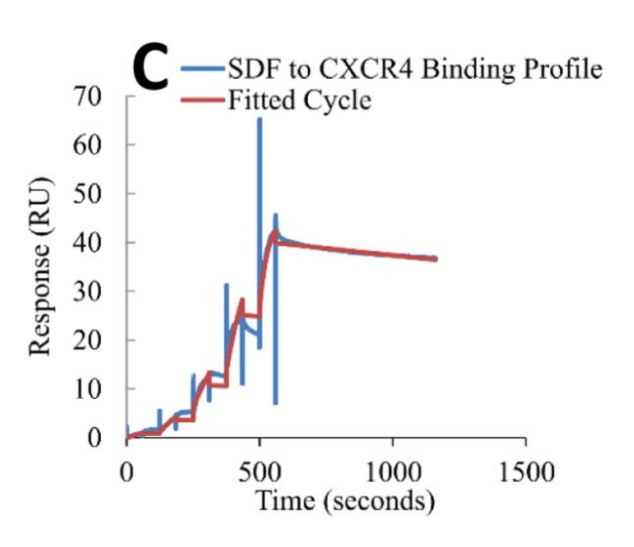
Fig3. Representative binding of free SDF1 to CXCR4 fitted sensogram. (Agnes Yeboah, 2016)
Related Resources
Immune diseases disorders are a class of complex diseases that affect the function of the human immune system. They can be caused by a variety of factors, including genetic factors, environmental exposures, lifestyle, and microbial infections. These disorders may involve overactivity of the immune system (such as autoimmune diseases), suppression of the immune system (such as immunodeficiency diseases), or an inappropriate response of the immune system to harmless substances (such as allergic reactions). The treatment of immune diseases usually requires a combination of management, including medication, lifestyle adjustments, and in some cases immunomodulatory therapy.
With the deepening of medical research, the understanding of immune diseases continues to increase, and treatments continue to advance. In the future, research into immune diseases may reveal new therapeutic targets and develop more personalized treatment options that offer hope to patients.
Contact us or send an email at for project quotations and more detailed information.
Quick Links
-

Papers’ PMID to Obtain Coupon
Submit Now -

Refer Friends & New Lab Start-up Promotions

