Fungal Infections Targets
🧪 HWP1-2705C
Source: Yeast
Species: Candida Albicans
Tag: His
Conjugation:
Protein Length: 27-203 aa

🧪 SAP2-4541C
Source: Yeast
Species: Candida albicans
Tag: His&Myc
Conjugation:
Protein Length: 57-398aa

🧪 SAP2-4542C
Source: E.coli
Species: Candida albicans
Tag: His
Conjugation:
Protein Length: 57-398aa

🧪 SAP6-4543C
Source: E.coli
Species: Candida albicans
Tag: His
Conjugation:
Protein Length: 77-418a

🧪 Asp f 1-30A
Source: E.coli
Species: Aspergillus fumigatus
Tag:
Conjugation:
Protein Length:

🧪 mitF-3722A
Source: E.coli
Species: Aspergillus fumigatus
Tag: His&Myc&SUMO
Conjugation:
Protein Length: 28-176aa

🧪 Lipase-3887R
Source: E.coli
Species: Rhizomucor miehei
Tag: His
Conjugation:
Protein Length: 25-363aa

🧪 Chitin-4044M
Source: E.coli
Species: Mucor rouxii
Tag: His
Conjugation:
Protein Length: 22-421aa

🧪 AspF2-01H
Source: E.coli
Species: Aspergillus Fumigatus
Tag: His
Conjugation:
Protein Length: 311

🧪 RFL8855PF
Source: E.coli
Species: Paracoccidioides brasiliensis
Tag: His
Conjugation:
Protein Length: Full Length (1-302)

🧪 RFL15940CF
Source: E.coli
Species: Candida albicans
Tag: His
Conjugation:
Protein Length: Full Length (1-385)

🧪 RFL5605CF
Source: E.coli
Species: Candida albicans
Tag: His
Conjugation:
Protein Length: Full Length (1-88)

🧪 RFL36939PF
Source: E.coli
Species: Paracoccidioides brasiliensis
Tag: His
Conjugation:
Protein Length: Full Length (1-309)

🧪 RFL30573NF
Source: E.coli
Species: Nectria haematococca
Tag: His
Conjugation:
Protein Length: Full Length (1-295)

Background
What are Fungal Infections?
Fungal infections are infections caused by fungi, which are organisms that live in soil, air and plants, and they can also live on the human body, for example on the skin. Fungal infections are usually spread by inhalation or contact with fungal spores, which can also land on the skin. People are more susceptible to fungal infections when their immune systems are weak or when they are on certain medications, such as cancer or organ transplant drugs. There are nearly 1-5 million species of fungi but only a few hundred can make people sick.
Fungal infections are passed when you inhale or come into contact with the spores from a fungus. The spores can also land on the skin. Some fungi can reproduce through spores. Fungal infections commonly start on the skin or in the lungs. Fungal infections range from mild to life-threatening. People with weakened immune systems (from illness, age, or medical treatments like steroids) are at higher risk for most fungal infections.
Symptoms of a fungal infection depend on the type and location of the infection and may include coughing, fatigue, headache, itchy skin, muscle pain, redness of the skin, and weight loss. Some fungal infections cause only skin-related symptoms, and these symptoms can be similar to other health problems, so it's important to talk to a medical provider and get a diagnosis.

What Causes Fungal Infections?
Many fungal diseases that are mild for most people can be life-threatening for people with certain risk factors. Some fungal diseases are only known to affect people with weakened immune systems. Common causes of fungal infections can be grouped into the following categories, including:
- Environmental factors
Moist and warm environments: Fungi prefer moist and warm environments, such as public bathrooms, swimming pools, gym locker rooms, etc.
Contact with sources of contamination: Contact with objects or surfaces contaminated with the fungus, such as public shower floors, shoes, towels, etc.
- Personal hygiene habits
Poor personal hygiene: not showering or changing clothes often, especially after sweating.
Skin damage: Small cuts or abrasions on the skin can be a route for fungal invasion.
- Reduced immune system function
Weak immune system: such as HIV/AIDS patients, cancer patients undergoing chemotherapy, patients using immunosuppressants, etc.
Chronic diseases such as diabetes and kidney disease may also increase the risk of infection.
- Drug use
Long-term use of antibiotics or corticosteroids: These drugs may disrupt the normal skin microbiota balance, giving the fungus a chance to overgrow.
- Age factor
Children and the elderly: Because their immune systems may not be as strong as adults', they are more susceptible to fungal infections.
- Genetic factors
Some people may be more susceptible to certain types of fungal infections because of genetic factors.
Some common fungi you can get infections from include:
- Dermatophytes. Dermatophytes are a group of fungi that live off of keratin, a substance in your hair, your nails and the outer layer of your skin. They don’t infect living tissue.
- Candida. Candida albicans is a yeast that naturally lives on your body, usually without causing problems. Under certain conditions, it can grow too much and cause itching and redness. Rarely, it can cause serious infections.
- Environmental fungi that live in soil or water. Examples include Histoplasma, Coccidioides, Blastomyces and Aspergillus.

What are the Types of Fungal Infections?
Fungal infections are usually spread by inhalation or contact with fungal spores. Spores can also land on the skin. Some fungi can reproduce by spores. Fungal infections usually start in the skin or lungs. Fungal infections vary in severity. Although millions of fungi exist, only a few pose a health problem. According to the location and severity of the infection, fungal infections can be divided into superficial fungal infections, subcutaneous fungal infections and deep fungal infections.
Superficial fungal infections affect the nails, skin and mucous membranes (such as the mouth, throat or vagina). For example, ringworm (dermatomycosis) is caused by fungi that live on the cells of the skin, hair, and nails (dermatomycosis). They can infect your feet (tinea pedis/athlete's foot), groin and inner thighs (jock itch/chafing), scalp (tinea capitis), hands (tinea capitis), facial hair and surrounding skin (tinea palpalis), and other body parts (tinea corporis). Candidiasis is an infection of the skin and mucous membranes (mucous membranes) caused by the bacteria Candida (usually Candida albicans), including oral thrush, certain types of diaper rash, vaginal yeast infection (vulvovaginitis), esophageal candidiasis, and intercandida. Tinea versicolor or pityriasis is a discoloration of the skin caused by the fungus Malassezia.
Subcutaneous fungal infections will get when a fungal entry into an incision or wound, usually through injury while working with plants (like a scratch from a thorn). They cause rashes, ulcers and other symptoms on your skin. Examples include: Sporotrichosis (rose gardener’s disease), Chromoblastomycosis and Eumycetoma.
Deep fungal infections can be found in places other than the skin of the body, such as the lungs, blood, urethra, or brain. Some are opportunistic infections, meaning they usually only cause illness in people with compromised immune systems. Deep or invasive fungal infections include: histoplasmosis, coccidioidomycosis (valley fever), blastomycosis, Aspergillosis, candida urinary tract infection, invasive candidiasis, pneumocystis pneumonia (PJP), and mucormycosis.
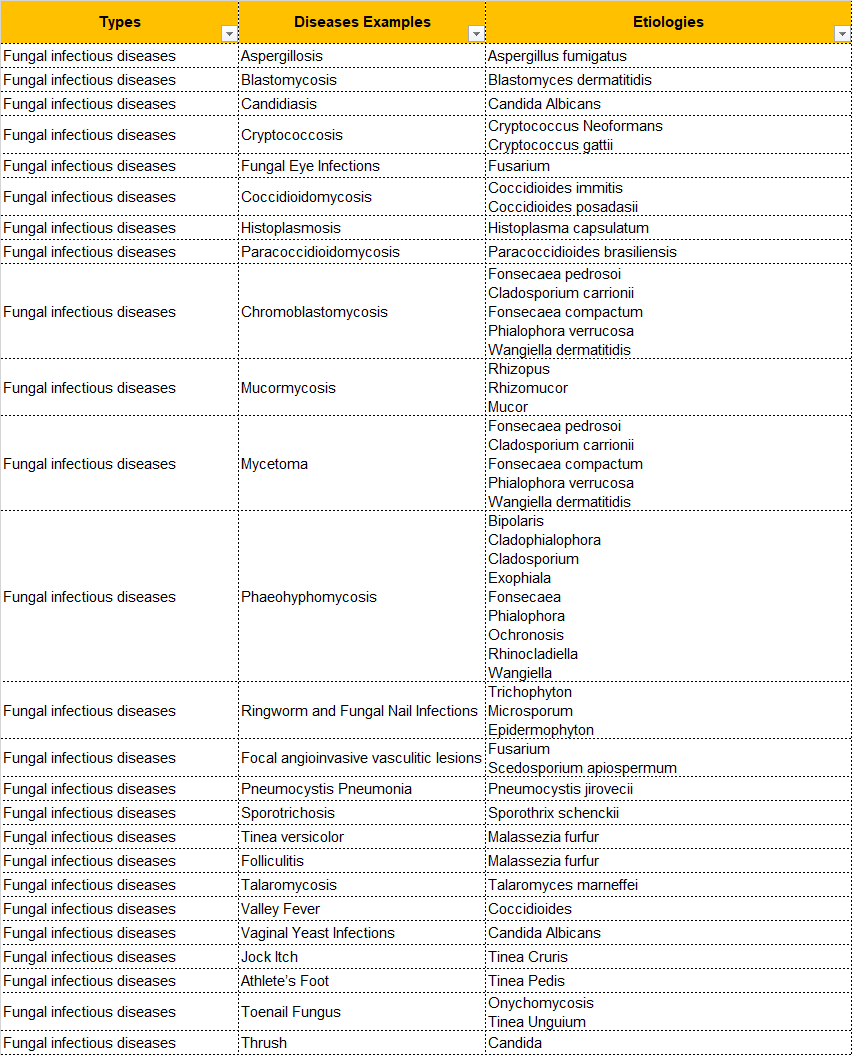
According to some common fungal infections, the types of these diseases and corresponding pathogenic fungi are listed.
Symptoms of Fungal Infections
Symptoms of fungal infections depend on what kind of fungal infection you have and where on your body it is. Symptoms are most common on your skin, nails or mucous membranes (like your mouth, throat or vagina). Sometimes you can have symptoms of an infection in your lungs, brain, eye, intestinal tract or sinuses. Generally speaking, symptoms of fungal infections may include:
- Coughing
- Fatigue
- Headache
- Itchy skin
- Muscle aches
- Skin redness
- Weight loss
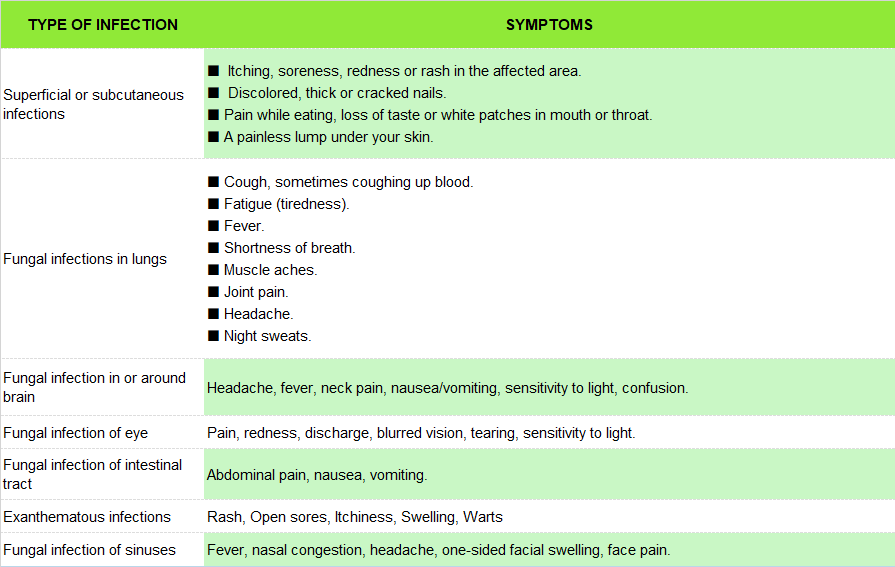
According to the symptoms of the disease site, the following disease symptoms are summarized.
How to Treat Fungal Infections?
Firstly, some suggestions for preventing fungal infections include thoroughly drying your skin, wearing waterproof shoes in public swimming pools and locker rooms, wearing breathable underwear (such as cotton materials), and if you are prone to infections such as beriberi, using a spray or powder to reduce the number of times an infection occurs. Many fungal infections can be cured with antifungal medication, which kills fungus in and on your body. What form of medication your healthcare provider prescribes depends on where the fungus is.
Treating fungal infections often requires tailoring treatment to the type, site, and severity of the infection, as well as the overall health of the patient. Here are some common treatments for fungal infections:
Local skin fungal infections: For local infections such as tinea pedis, tinea corporis, and tinea jock, topical treatments are often recommended, including over-the-counter medications such as ointments, creams, powders, and sprays. For example, topical medications such as bibenzazole, miconazole nitrate, and terbinafine need to be used continuously for four weeks, applied 1-2 times daily, and continued for two weeks after the rash has subsided.
Oral antifungals: For severe or difficult-to-treat skin fungal infections, oral antifungals such as itraconazole or terbinefin may be required. In addition, for onychomycosis, oral medications are often more effective than topical treatments.
Pulmonary fungal infections: Treatment may include fluconazole, itraconazole, echinocin like carpofungin or micafungin, and amphotericin B. The choice of specific drugs depends on the severity of the infection and the resistance of the pathogen.
Invasive fungal infections: In patients with acute leukemia, treatment of invasive fungal infections may require the use of higher grade antifungal drugs and switching to oral therapy after symptoms improve. Ensuring adequate drug exposure and monitoring the effects of treatment are key to treatment.
Non-pharmacological treatments: Good skin care, including regular bathing and keeping the skin dry, is fundamental to preventing fungal skin infections. Avoid walking barefoot in public bathrooms and showers, wear breathable shoes and absorbent socks, and use powder to control humidity.
Special treatment for tinea capitis: Tinea capitis may require the use of an antifungal shampoo as an adjunct treatment, and avoid sharing personal items that may be contaminated.

Case Study
Case Study 1: Recombinant Human CYP51A
MICs of most antifungals in clinical use are elevated against A. lentulus, and it shows primary resistance to azole drugs. Two A. lentulus cytochrome P450 14-α sterol demethylases, encoded by A. lentulus cyp51A (Alcyp51A) and Alcyp51B genes, were identified. Targeted cyp51A gene knockout in A. lentulus showed that the intrinsic azole resistance of this species is cyp51A dependent. The Δcyp51A strain was morphologically indistinguishable from the A. lentulus wild-type strain, retaining the ability to cause pulmonary disease in neutropenic mice. The heterologous expression of A. lentulus cyp51A was performed in an A. fumigatus cyp51A-deficient strain, confirming that Cyp51A is responsible for the differences in A. lentulus-azole drug interaction.
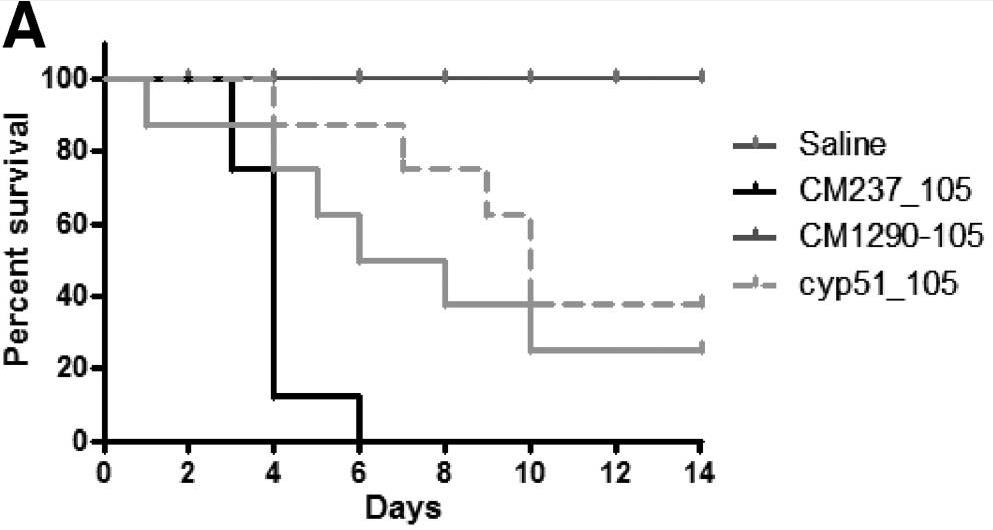
Fig1. Comparative analysis of the survival of CD-1 immunocompromised mice infected with the A. fumigatus. (Emilia Mellado, 2011)
Case Study 2: Recombinant membrane-integrated synthase FKS
FKS is the target of widely prescribed antifungal drugs. Unfortunately, the mechanism of action of FKS remains enigmatic and this has hampered development of more effective medicines targeting the enzyme. Here researchers present the cryo-electron microscopy structures of Saccharomyces cerevisiae FKS1 and the echinocandin-resistant mutant FKS1(S643P). These structures reveal the active site of the enzyme at the membrane-cytoplasm interface and a glucan translocation path spanning the membrane bilayer. Multiple bound lipids and notable membrane distortions are observed in the FKS1 structures, suggesting active FKS1-membrane interactions. Echinocandin-resistant mutations are clustered at a region near TM5-6 and TM8 of FKS1. The structure of FKS1(S643P) reveals altered lipid arrangements in this region, suggesting a drug-resistant mechanism of the mutant enzyme.
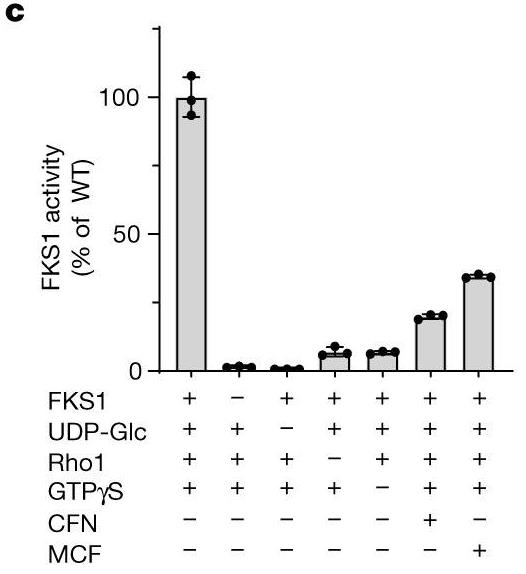
Fig2. In vitro activity of CHAPS-purified FKS1 with different effectors. (Xinlin Hu, 2023)
Case Study 3: Recombinant Ras-GAP protein
- fumigatus must adapt to hypoxic microenvironments to survive and thrive in human lungs. To gain further insights into hypoxic adaptation, researchers generated a laboratory-evolved strain (Afs35-G20) harboring hypoxia fitness, and identified a nonsense mutation in AfgapA encoding a Ras-GAP protein, which could result in the deletion of 22 amino acids at the C-terminus. They investigated the role of AfgapA in hypoxia fitness by constructing Afs35-G20-AfgapAWT, and ∆AfgapA. Indeed, the hypoxia fitness of Afs35-G20 was reversed by introducing AfgapAWT. ∆AfgapA exhibited greater hypoxia fitness and hypervirulence in the silkworm infection model, indicating that AfgapA is responsible for hypoxia fitness, particularly in liquid cultures.
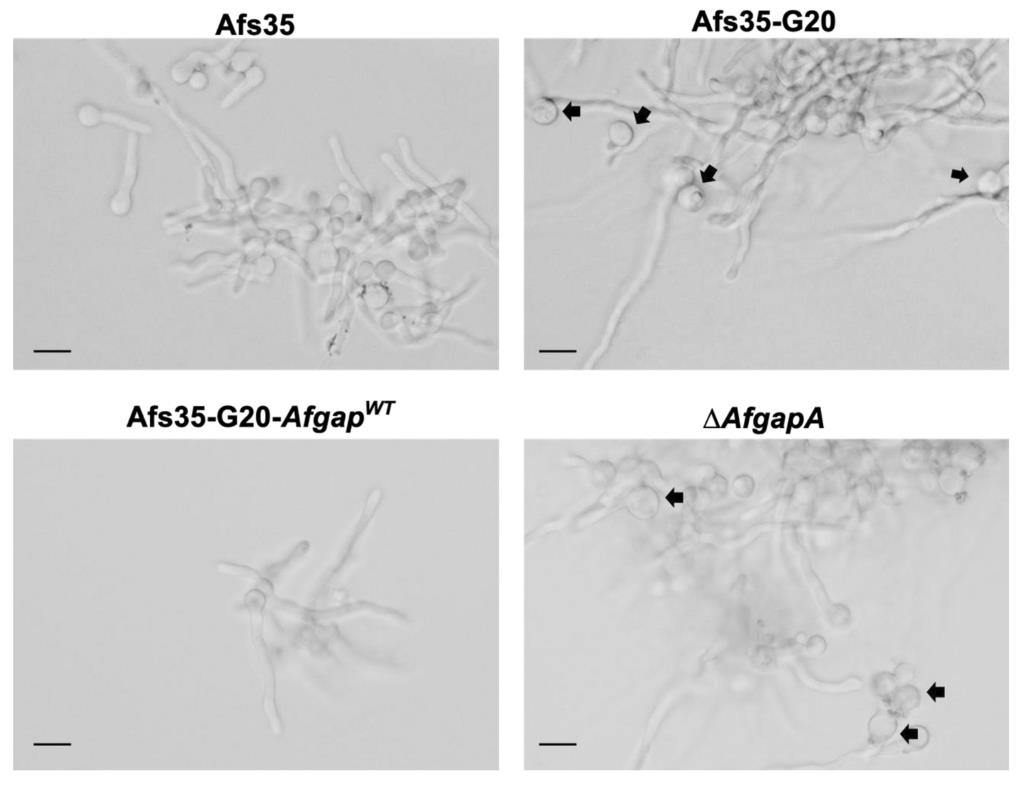
Fig3. Effect of AfgapA on conidia morphology during germination. (Cai Bian, 2022)
Related Resources
Fungal infections vary. Although there are millions of types of fungi, only a few cause problems for your health. Symptoms of these infections vary, but many types of fungal infections cause skin symptoms like an itchy rash, cracked skin, or red skin. Fungal infections often have OTC treatments, but some require prescription medication. Researchers are also continuing to work on drug treatment options for common infections or more severe types to benefit patients.


