What is CD19 Protein
The CD19 protein, officially known as Cluster of Differentiation 19, stands as a pivotal player in the realm of immunology. Also recognized by synonyms such as B4, CVID3, and MGC12802, CD19 is a key member of the immunoglobulin superfamily. In this article, we delve into the intricacies of CD19, from its structural characteristics to recent research advances, shedding light on its diverse functions, associated diseases, signal pathways, and promising applications in the biomedical field.
CD19 Protein Structural Characteristics and Classification
CD19, belonging to the immunoglobulin superfamily, is encoded by the CD19 gene located on chromosome 16 in humans. Structurally, it comprises extracellular domains with immunoglobulin-like loops, a transmembrane domain, and a cytoplasmic tail. Classified as a type I transmembrane protein, CD19 serves as a critical co-receptor for B cell activation and differentiation.
Recent Research Advances about CD19 Protein
Recent research has unveiled the multifaceted role of CD19 in immune responses. Scientists have explored the dynamic interaction of CD19 with other B cell receptors and its impact on signal transduction pathways. The discovery of novel CD19 isoforms has sparked interest, suggesting a deeper complexity in its functional diversity. Additionally, cutting-edge technologies like CRISPR have enabled precise manipulation of CD19, opening avenues for targeted therapeutic interventions.
CD19 Biological Functions and Molecular Mechanisms
CD19 plays a central role in B cell development and activation. Acting as a co-receptor alongside the B cell receptor (BCR), CD19 amplifies B cell responses to antigens. Its involvement in signal transduction pathways, such as the PI3K-Akt pathway, regulates key processes like proliferation, survival, and antibody production. CD19's intricate dance with other signaling molecules orchestrates a harmonious immune response against invading pathogens.
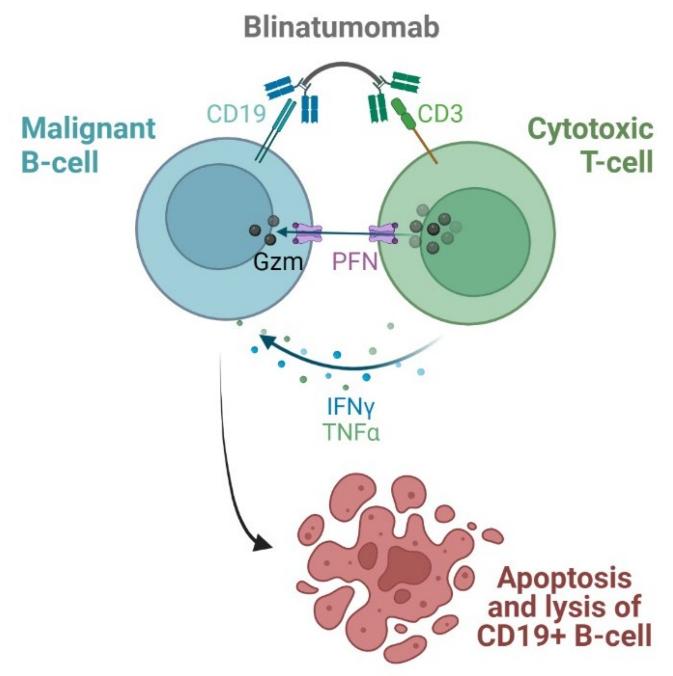
Figure 1. Blinatumomab mechanism of action. (Sochacka-Ćwikła A, et al., 2021)
CD19 Related Signaling Pathway
The CD19 signal pathway is a complex network of molecular interactions that govern B cell activation. Upon antigen recognition, CD19 collaborates with the BCR to initiate a cascade of signaling events. Notably, CD19's role in activating the PI3K-Akt pathway enhances B cell survival and proliferation. Elucidating the nuances of these pathways not only enhances our understanding of basic immunology but also holds promise for targeted therapeutic interventions.
CD19 Related Diseases
The dysregulation of CD19 expression or function has been linked to various diseases, primarily those affecting the immune system. Notably, CD19 deficiency is associated with Common Variable Immunodeficiency 3 (CVID3), a primary immunodeficiency disorder characterized by recurrent infections. Furthermore, aberrant CD19 expression is implicated in B cell malignancies, such as B cell lymphomas and leukemias, highlighting its significance in cancer biology.
CD19's Applications in Biomedicine
Harnessing the unique properties of CD19 has paved the way for innovative applications in the biomedical field. In diagnostic development, CD19 serves as a valuable marker for B cell-related disorders. Its presence or absence can be indicative of immune system health, aiding in the diagnosis of immunodeficiencies or malignancies. Additionally, CD19 is a focal point in vaccine development efforts, aiming to bolster B cell responses against specific pathogens.
In therapeutics, CD19 has emerged as a target for immunotherapy, particularly in the context of B cell malignancies. Chimeric Antigen Receptor T-cell (CAR-T) therapies that target CD19 have shown remarkable success in treating certain forms of leukemia and lymphoma. These groundbreaking developments underscore the pivotal role CD19 plays in advancing therapeutic strategies for challenging diseases.
Recommended Products
| Cat.# | Product name | Species | Source (Host) | Tag |
|---|---|---|---|---|
| CD19-315C | Recombinant Cynomolgus CD19 Protein, Fc-tagged | Cynomolgus | HEK293 | Fc |
| CD19-1075C | Recombinant Cynomolgus CD19 Protein (Met1-Lys292), His-tagged | Cynomolgus | HEK293 | His |
| CD19-3309HAF555 | Recombinant Human CD19 Protein, His-tagged, Alexa Fluor 555 conjugated | Human | HEK293 | His |
| CD19-3308HAF647 | Active Recombinant Human CD19 Protein, Fc-tagged, Alexa Fluor 647 conjugated | Human | HEK293 | Fc |
| CD19-408HAF488 | Recombinant Human CD19 Protein, Fc-tagged, Alexa Fluor 488 conjugated | Human | HEK293 | Fc |
| CD19-408HAF555 | Recombinant Human CD19 Protein, Fc-tagged, Alexa Fluor 555 conjugated | Human | HEK293 | Fc |
| CD19-3307HF | Active Recombinant Human CD19 Protein, Fc-tagged, FITC conjugated | Human | HEK293 | Fc |
| D19-3307HP | Recombinant Human CD19 protein, Fc-tagged, R-PE labeled | Human | HEK293 | Fc |
| CD19-280H | Recombinant Human CD19, Fc-tagged, Biotinylated | Human | HEK293 | Fc |
| CD19-3308HP | Recombinant Human CD19 protein, Fc-tagged, R-PE labeled | Human | HEK293 | Fc |
Reference
- Sochacka-Ćwikła A, et al. FDA-approved drugs for hematological malignancies—The last decade review. Cancers. 2021, 14(1): 87.

