Protocol of Immobilized Metal Affinity Chromatography
In addition to the enrichment of phosphorylated proteins, phosphorylated peptides can also be enriched. There are many ways to enrich phosphorylated peptides. Immobilized metal affinity chromatography (IMAC) was first proposed by Porath in 1975. After decades of development, it has become the most popular method for the separation and analysis of phosphorylated peptides, and is also a relatively mature technology for the separation and enrichment of phosphorylated peptides. It uses the high affinity of phosphate groups and solid metal ions such as Fe3+, Ga2+ and Cu2+ to enrich the phosphorylated peptide segments. In addition, those non-phosphorylated peptides rich in acidic amino acids also have the ability to bind to solid metal ions, and may also be enriched. The disadvantage is that some phosphorylated peptides with weak binding ability to IMAC column or some phosphorylated peptides that are difficult to elute due to multiple phosphorylation sites may be lost. In addition, the affinity of TiO2 with the phosphate group on the phosphorylated peptide segment can be used to realize the relative enrichment of phosphate peptides.
At present, the high throughput phosphorylated proteome analysis mainly adopts the method of IMAC affinity chromatography-reversed-phase liquid chromatography-tandem mass spectrometry - database retrieval. The advantage of this method is that each soluble phosphorylated peptide segment, regardless of its length, can be enriched, and the sample eluted by IMAC column can be directly combined with LC for subsequent MOLD-TOF/TOF mass spectrometry identification. The enriched peptide segment can also be further analyzed by two-dimensional acid bump peptide (2D-PP). This method provides important information about protein phosphorylation state that other methods cannot provide, including:
(1) The maximum number of phosphorylation sites;
(2) The autoradiography intensity provides the relative stoichiometry of phosphorylation in all phosphorylated peptides;
(3) The orthogonal separation of electrophoresis and thin layer chromatography provides the relative state of hydrophilicity between phosphate peptides.
The purified phosphorylated peptide generated by 2D-PP map can be directly used for MS analysis after extraction. In addition, 2D-PP atlas has high sensitivity and good reproducibility. However, if the 2D-PP map is used as the preparation method for MS/MS analysis, the added protease should be as little as possible, because when the excessive protease is used for MS analysis of phosphate pus, its self-cutting products will occupy the dominant position of the map and inhibit the analysis signal of phosphate peptide.
This lab manual is designed to help researchers master the basic principles and main steps of enrichment of phosphorylated peptides by solid-phase metal ion affinity chromatography and understand the methods and applications of enrichment of phosphorylated peptides by solid-phase metal ion affinity chromatography.
This section mainly introduces the enrichment of phosphorylated peptides by solid phase metal ion affinity chromatography. Because the solid phase metal affinity chromatography (IMAC) uses the high affinity of phosphate groups and solid metal ions such as Fe3+, Ga2+ and Cu2+ to enrich phosphorylated peptides, this binding ability is affected by pH, ionic strength and organic phase of solution. In the buffer solution with high pH or phosphate, the binding between metal ions and phosphate groups is destroyed, and the phosphorylated peptides are released. IMAC method is fast and direct, and the sample enriched by IMAC can be directly used for mass spectrometry analysis after desalting. Here we take the photos-photoprotein enrich kit as an example to introduce it.
At present, IMAC technology is often combined with LC-MS/MS, which enables IMAC technology to be applied to the study of phosphorylated proteome. The peptide segments were separated by using organic and inorganic phases of different concentrations, and then spotted on the target for mass spectrometry analysis; Or it can be separated and tested by 2D-PP. When using this method, the samples are labeled with radioactive markers, and the thin layer fiberboard principle is always used for separation; The second direction is separated by thin layer chromatography (TCL) based on the principle of adsorption chromatography.
1. Main Instruments and Equipment
Micro-pipette, centrifuge tube, constant temperature water bath, rotary evaporator, LC-high pressure liquid phase, centrifuge, ion exchange column, thin layer fiberboard, electrophoresis device, autoradiography device.
2. Material
Total protein extracted by various methods and protein samples labeled with 32P.
3. Main reagents
(1) Enrichment kit: PHOS-TRAPTM photosoprotein enrichment kit.
(2) 2D Clean-up kit.
(3) 2D-Quant kit.
(4) Sample dissolution: 0.5mol/L triethylammonium bicarbonate (pH8.5).
(5) Denatured solution: 2% SDS.
(6) Reduction reagent TCEP.
(7) Blocking buffer: 84mmol/L iodoacetamide.
(8) Trypsin 0.1μ g/ μ L.
(9) 2D-PP reagent.
1. 2D Clean-up kit purifies proteina
2. 2D Quant kit to determine protein concentration
3. Enzymatic digestion of protein samples
(1) Take 100μg of dried sample powder and add 20μL of the dissolution solution to a final protein concentration of 5μg/μL.
(2) Add 1μL of denaturing solution and vortex shake

(3) Add 1μL of reducing reagent (TCEP) to its final concentration of 5 mmol/L and vortex shake.
(4) Incubate at 60°C for 1h.
(5) Centrifuge the sample, add 1μL of freshly prepared 84 mmol/L iodoacetamide*1, vortex shake, and leave at room temperature for 30 min.
(6) After centrifugation, add 20μL trypsin (0.1μg/μL)*2 and vortex shake.
(7) Digest the samples overnight (12-16h) at 37°C.
4. Phos-trapTMMagnetic Beads
(1) Take 380μL of deionized water*3 in a 50mL centrifuge tube, add 20μL of enriched magnetic beads*4, and mix gently.

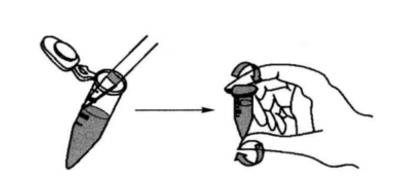
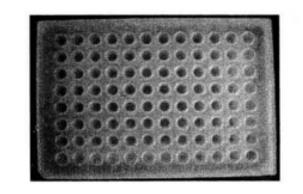
(2) Transfer 200μL of the mixture to a 96-well plate, and then transfer the 96-well plate to a magnetic bead rack for 1 min. the beads will collect to the bottom of the tube.
(3) Remove the supernatant, remove the 96-well plate from the magnetic bead rack, add 200μL of binding buffer*5, mix gently, and move the 96-well plate to the magnetic bead rack for 1min.
(4) The beads will gather to the bottom of the tube (repeat more than 2 times).
5. Phosphorylated peptide enrichment
In order to separate phosphorylated protein as much as possible, we use a 24cm adhesive strip, pH 3~11, and the sample loading amount is 150μg. Perform two-dimensional electrophoresis.
(1) Add 430μL binding buffer to 43μL of the finished sample to dilute the sample*6 and mix well. Add to the equilibrated enrichment magnetic beads and mix well.
(2) Place on the mixer at room temperature for 10 min, then place on the magnetic bead rack for 1 min and remove the supernatant.
(3) Add 200μL binding buffer, fully suspend and wash the beads. Place on the bead rack for 1 min and remove the supernatant (repeat more than 3 times).
(4) Add 200μL wash buffer*7, mix well and wash, then place on the magnetic bead rack for 1min and remove the supernatant.
(5) Add 20μL of elution buffer, mix at room temperature for 5 min on a mixer, then place on the bead rack for 1 min, and collect the supernatant containing the phosphorylated peptide.
6. Analysis and detection of phosphorylated peptides
(1) If the protein has not been labeled prior to separation, select the appropriate mobile phase for LC separation of the peptide.
Mix matrix spot targets after separation.
(2) If the protein has been radiolabeled, 2D-PP assay can be performed.
① Prepare a thin fiber plate.
② Dispense the sample solution with a capillary tube at one end of the thin layer plate, place it in a closed bath and add a suitable solvent as the mobile phase.
③ One-way electrophoresis separation.
④ In two-way electrophoresis, according to the capillary principle, the solvent is sucked up and moved along the plate and drives the components of the sample forward, a process called unfolding.
⑤ Due to the different nature of each component, the moving distance is different, and after unfolding a certain distance, the component spots that are separated from each other are obtained.
⑥ Radiographic autofluorescence detection signal*8.
1. When solubilizing proteins, care should be taken to mix the reagents well after each addition so that the reagents can fully interact with the proteins. Get a completely linear amino acid molecule, which helps the smooth progress of enzymatic digestion.
2. Protein reduction before the process of enzymatic digestion, protein denaturation should be sufficient, otherwise it will affect the subsequent operation.
3. The amount of enzyme and processing time should be suitable for the protein enzymatic digestion process.
4. The magnetic bead adsorption time etc. should be adequate during the enrichment process. The whole operation should be meticulous and gentle to avoid the magnetic beads being sucked away and taking away the phosphorylated peptides.
5. After the phosphorylated peptide is enriched, a suitable method should be selected for separation and identification.
*1 Iodoacetic acid carboxymethylates sulfhydryl groups and prevents cysteine degradation.
*2 In general, enzyme volume: protein volume = 1:50.
*3 Deionized water volume (μ) = (number of fractions + 1) × 190.
*4 Enriched magnetic beads volume (μ) = (number of fractions + 1) × 10.
*5 When pipetting the liquid containing enriched magnetic beads, try to use a 1mL tip to avoid damage to the surface of magnetic beads.
*6 When using the binding buffer for the first time, add 100mL of chromatographic grade acetonitrile.
*7 When using wash buffer for the first time, add 25mL of chromatographic grade acetonitrile.
*8 The maximum number of phosphorylation sites can be seen from the results; the intensity of the radioautography provides the relative stoichiometry of phosphorylation in all phosphorylated peptide segments.

