Tissue Regeneration
Creative BioMart Tissue Regeneration Product List
Immunology Background
Background
Tissue regeneration is the process by which damaged or injured tissues in the body are replaced and repaired to restore normal function. This process is vital for maintaining the health and integrity of organs and tissues in the body. Tissue regeneration can occur through various mechanisms, such as cell proliferation, differentiation, and migration.
Tissue regeneration markers are specific molecules or substances that are involved in the regulation and coordination of the tissue regeneration process. These markers can be proteins, genes, cells, or other biological factors that indicate the presence of tissue repair and regeneration. By studying and monitoring these markers, researchers can gain insights into the mechanisms underlying tissue regeneration and develop strategies to promote and enhance the regenerative capacity of the body.
Tissue regeneration markers play a crucial role in identifying the types of cells involved in the regeneration process, tracking the progression of tissue repair, and evaluating the effectiveness of regenerative therapies. They can also serve as diagnostic tools for assessing the extent of tissue damage and predicting the outcome of regeneration in various diseases and injuries.
Overall, understanding tissue regeneration markers is essential for advancing regenerative medicine and developing new therapies for a wide range of medical conditions, including wound healing, tissue injuries, and degenerative diseases. By harnessing the power of these markers, researchers can pave the way for innovative treatments that harness the body's natural regenerative capacity to restore health and function to damaged tissues.
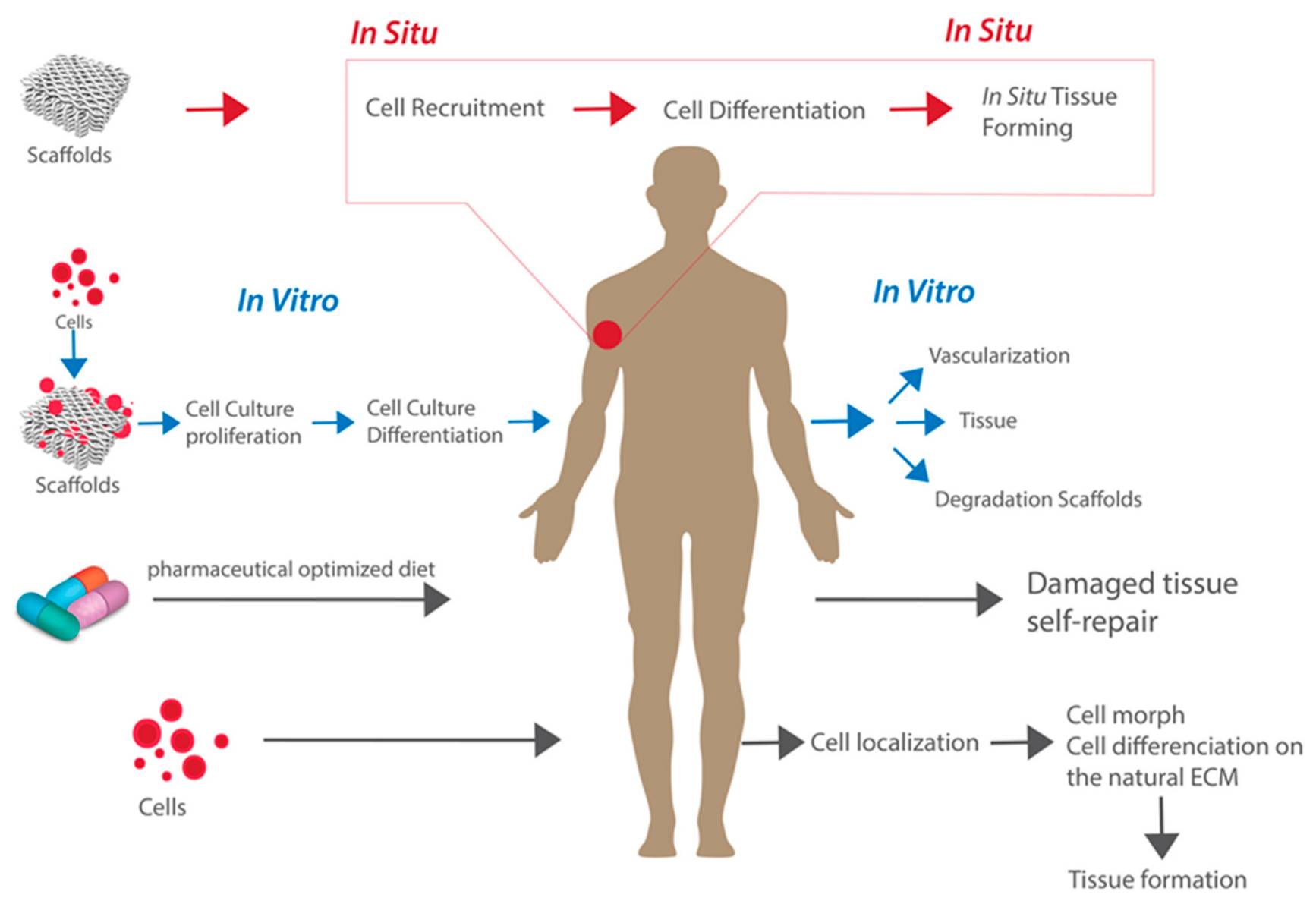 Fig.1 Pathways for tissue regeneration. (Abdulghani S, et al., 2019)
Fig.1 Pathways for tissue regeneration. (Abdulghani S, et al., 2019)The Significance of Studying Tissue Regeneration Markers
Studying markers of tissue regeneration holds immense significance in the fields of regenerative medicine, tissue engineering, and biomedical research. Here are some key reasons why the investigation of tissue regeneration markers is crucial:
| Significance | Details |
|---|---|
| Understanding Regenerative Processes | By studying markers of tissue regeneration, researchers can gain valuable insights into the molecular and cellular mechanisms that drive tissue repair and regeneration. This knowledge is essential for developing targeted interventions to enhance the body's natural healing processes. |
| Identification of Stem Cells and Progenitor Cells | Tissue regeneration markers can help identify specific cell populations with stem cell or progenitor cell properties that are crucial for tissue repair. Understanding these markers aids in isolating and characterizing these regenerative cell populations for therapeutic applications. |
| Predicting Regenerative Potential | Biomarkers associated with tissue regeneration can serve as indicators of the regenerative potential of tissues and organs. Monitoring the expression of these markers can help predict the capacity of a tissue to repair itself and guide treatment strategies for optimal outcomes. |
| Development of Regenerative Therapies | Insights gained from the study of tissue regeneration markers are essential for the development of regenerative therapies. By targeting specific markers or signaling pathways, researchers can design novel treatments to promote tissue repair, reduce scarring, and restore tissue function. |
| Personalized Medicine | Understanding tissue regeneration markers enables the development of personalized regenerative medicine approaches. By analyzing an individual's unique marker profile, clinicians can tailor treatment plans to the specific regenerative needs of each patient, leading to more effective and targeted interventions. |
| Diagnostic and Prognostic Tools | Tissue regeneration markers can serve as diagnostic and prognostic tools for assessing the extent of tissue damage, monitoring healing progress, and predicting patient outcomes. Biomarker-based assays can provide valuable information for healthcare providers to make informed clinical decisions. |
In summary, studying markers of tissue regeneration is essential for advancing our understanding of regenerative processes, developing innovative therapies, and improving patient care in various medical settings. The insights gained from such research have the potential to revolutionize the field of regenerative medicine and lead to novel treatments for tissue injuries, degenerative diseases, and organ transplantation.
Different Types of Tissue Regeneration Markers
Classification 1
Tissue regeneration markers play a crucial role in identifying and characterizing different types of stem cells involved in tissue repair and regeneration. Two main types of stem cells are adult/somatic stem cells and embryonic and induced pluripotent stem cells, each with specific markers that can be used for their identification.
| Types | Features |
|---|---|
| Adult/Somatic Stem Cells Markers |
|
| Embryonic and Induced Pluripotent Stem Cells Markers |
|
These markers are used in research and clinical settings to isolate and characterize different types of stem cells, monitor their differentiation potential, and track their behavior during tissue regeneration processes. Understanding the expression of these markers is essential for advancing regenerative medicine and developing new therapeutic strategies for tissue repair and regeneration.
Classification 2
Tissue regeneration markers play a crucial role in the process of tissue repair and regeneration by promoting cellular proliferation, differentiation, and tissue remodeling. These markers also can be broadly categorized into growth factors, cytokines, and extracellular matrix proteins.
| Types | Features |
|---|---|
| Growth Factors |
Growth factors are signaling molecules that regulate various cellular processes such as cell growth, proliferation, and differentiation. They play a key role in tissue regeneration by promoting cell migration and proliferation, enhancing angiogenesis, and stimulating the production of extracellular matrix components. Some of the important growth factors involved in tissue regeneration include:
|
| Cytokines |
Cytokines are small proteins that regulate immune responses and inflammatory processes in the body. They also play a crucial role in tissue regeneration by modulating cellular communication and signaling pathways. Some of the key cytokines involved in tissue regeneration include:
|
| Extracellular Matrix Proteins |
Extracellular matrix proteins provide structural support and promote cell adhesion, migration, and differentiation during tissue regeneration. Some commonly studied extracellular matrix proteins include:
|
Methods Used to Detect and Quantify Tissue Regeneration Markers
Detection and quantification of tissue regeneration markers in biological samples typically involve a combination of molecular biology techniques, immunoassays, and imaging methods. Here are some commonly used methods for detecting and quantifying tissue regeneration markers:
| Methods | Details |
|---|---|
| Immunohistochemistry (IHC) |
Principle: IHC involves the use of antibodies to detect specific proteins within tissue samples. Procedure: Tissue sections are treated with primary antibodies against the target regeneration markers, followed by secondary antibodies conjugated to a detection molecule (e.g., enzyme or fluorophore). Detection: Visualization of antibody binding is achieved through colorimetric, fluorescent, or enzymatic reactions, allowing for the localization and semi-quantification of the markers within the tissue. |
| Western Blotting |
Principle: Western blotting is used to detect and quantify specific proteins in a sample based on their molecular weight. Procedure: Proteins are separated by gel electrophoresis, transferred to a membrane, and probed with antibodies against the regeneration markers of interest. Detection: The bound antibodies are visualized using chemiluminescence or colorimetric methods, providing information on the presence and relative abundance of the markers. |
| Enzyme-Linked Immunosorbent Assay (ELISA) |
Principle: ELISA is a quantitative immunoassay that utilizes enzyme-conjugated antibodies to detect and quantify specific proteins in a sample. Procedure: Samples are incubated in microplate wells coated with capture antibodies specific to the regeneration markers. Detection antibodies labeled with enzymes are added, and a substrate is used to produce a measurable signal. Detection: The intensity of the signal is proportional to the concentration of the markers in the sample, allowing for quantitative analysis. |
| Quantitative Polymerase Chain Reaction (qPCR) |
Principle: qPCR is used to quantify the expression levels of genes associated with tissue regeneration markers. Procedure: RNA is extracted from the sample, converted to cDNA, and amplified using specific primers targeting the genes of interest. Detection: Fluorescent dyes or probes are used to monitor the accumulation of PCR products in real-time, providing quantitative data on gene expression levels. |
| Flow Cytometry |
Principle: Flow cytometry is a technique used to analyze and quantify specific proteins on the surface of cells. Procedure: Cells are labeled with fluorescently-conjugated antibodies against the regeneration markers and analyzed as they pass through a flow cytometer. Detection: By measuring the fluorescence intensity of individual cells, flow cytometry enables the quantification of marker expression on a cell-by-cell basis. |
| Immunofluorescence Microscopy |
Principle: Immunofluorescence microscopy allows for the visualization and quantification of proteins within cells or tissues using fluorescently-tagged antibodies. Procedure: Samples are incubated with fluorescently-labeled antibodies against the regeneration markers, and imaging is performed using a fluorescence microscope. Detection: The intensity and localization of fluorescence signal provide information on the distribution and expression levels of the markers. |
| Mass Spectrometry |
Principle: Mass spectrometry is a powerful technique used for the identification and quantification of proteins in biological samples. Procedure: Proteins are digested into peptides, which are then analyzed by mass spectrometry to determine the presence and abundance of the regeneration markers. Detection: Mass spectrometry generates mass spectra that can be used to identify specific proteins and quantify their levels in the sample. |
These methods offer diverse approaches for detecting and quantifying tissue regeneration markers in biological samples, providing valuable insights into the molecular mechanisms underlying tissue repair and regeneration. Researchers often employ a combination of these techniques to comprehensively analyze the expression and localization of specific markers in various experimental contexts.
Case Study
Case 1: Abbas TO, Mahdi E, Hasan A, AlAnsari A, Pennisi CP. Current status of tissue engineering in the management of severe hypospadias. Front Pediatr. 2018;5:283.
Hypospadias is a common birth defect in male children where the urinary opening is misplaced on the underside of the penis. Current surgical techniques for repair are not universally effective due to the variability in anatomical presentation. Complications post-surgery are high, especially in severe cases, and require experienced surgeons. Tissue engineering techniques are being developed to simplify procedures and reduce complications, using biomaterials such as synthetic and natural polymers that may be seeded with cells. While some success has been seen in preclinical and clinical studies, a universally effective tissue engineering approach for hypospadias repair is still being sought.
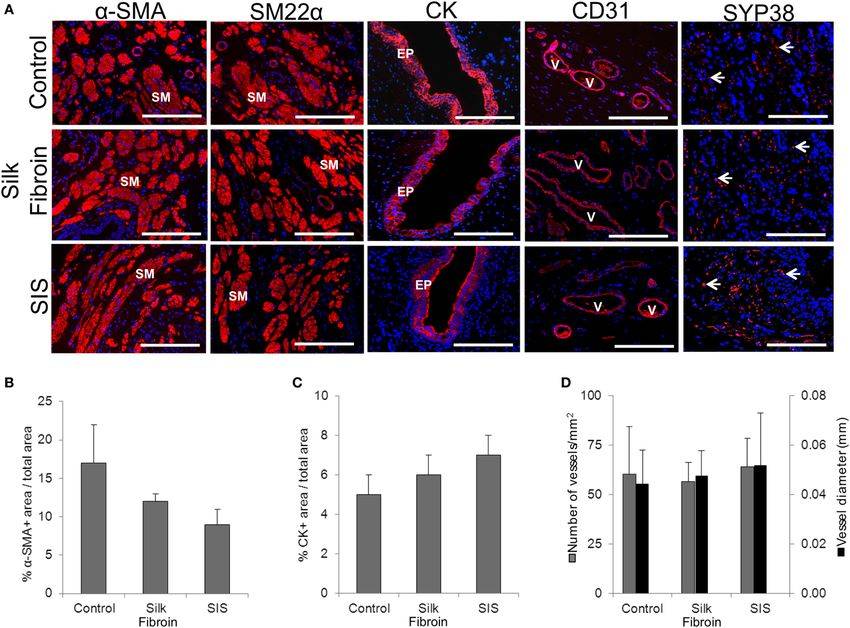 Fig.1 Urethral tissue regeneration following implantation of acellular silk fibroin scaffolds in rabbits.
Fig.1 Urethral tissue regeneration following implantation of acellular silk fibroin scaffolds in rabbits.
(A) Immunohistochemical assays showed expression of smooth muscle contractile markers, epithelial-associated cytokeratins, and endothelial markers. (B-D) The panels displayed histomorphometric data from alpha-smooth muscle actin positive regions, cytokeratin positive cells, and CD31 positive vessels obtained from control and scaffold implanted animals. The results suggest that the scaffold implantation stimulated the expression of these markers in the tissue.
Case 2: Chen K, Kwon SH, Henn D, et al. Disrupting biological sensors of force promotes tissue regeneration in large organisms. Nat Commun. 2021;12(1):5256.
In this study, the researchers examined the effects of blocking mechanotransduction on tissue repair in large animals by using a specific inhibitor of FAK (FAKI) in red duroc pigs. FAKI was delivered to wounds in a controlled manner using a biodegradable hydrogel scaffold. They found that wounds treated with FAKI healed significantly faster and with less scar formation compared to standard dressings or empty hydrogels. Additionally, the treated skin had better elasticity and biomechanical properties similar to unwounded skin. Overall, blocking mechanical signaling with FAKI resulted in improved wound healing outcomes in pigs.
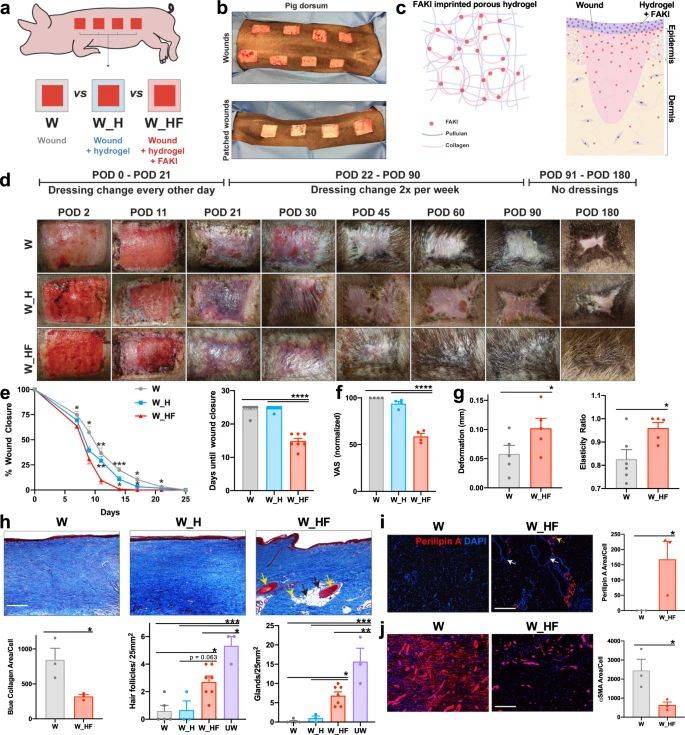 Fig.2 Disruption of mechanotransduction in large organisms accelerates deep partial-thickness wound healing, attenuates fibrotic scar formation, and promotes tissue regeneration.
Fig.2 Disruption of mechanotransduction in large organisms accelerates deep partial-thickness wound healing, attenuates fibrotic scar formation, and promotes tissue regeneration.Related References
- Kostereva NV, Wang Y, Fletcher DR, et al. IGF-1 and chondroitinase ABC augment nerve regeneration after vascularized composite limb allotransplantation. PLoS One. 2016;11(6):e0156149.
- Abdulghani S, Mitchell GR. Biomaterials for in situ tissue regeneration: a review. Biomolecules. 2019;9(11):750.

