What is CD40 Protein
The CD40 protein, formally known as Cluster of Differentiation 40, is a transmembrane receptor glycoprotein that plays a pivotal role in the immune system. Also referred to as TNFRSF5 (Tumor Necrosis Factor Receptor Superfamily Member 5), CD40 is a member of the TNF receptor superfamily. Structurally, it boasts a characteristic cysteine-rich domain, facilitating its classification within the tumor necrosis factor receptor superfamily (TNFRSF). Recent advancements in research have shed light on the intricate details of CD40, unveiling its significance in orchestrating immune responses.
CD40 Biological Functions and Molecular Mechanisms
CD40 is a linchpin in the intricate web of immune responses. Its biological functions are vast and pivotal for the proper functioning of the immune system. The primary role of CD40 is to serve as a co-stimulatory molecule, bridging the communication between antigen-presenting cells, such as dendritic cells, and B cells. This interaction is vital for the initiation and regulation of immune responses.
At the molecular level, CD40 engages in complex interactions with its ligand, CD40L (CD154), predominantly expressed on activated T cells. This binding activates a cascade of signaling events, triggering the expression of cytokines, chemokines, and adhesion molecules. The CD40-CD40L axis is crucial for the formation of immunological synapses, ensuring effective communication and coordination among immune cells.
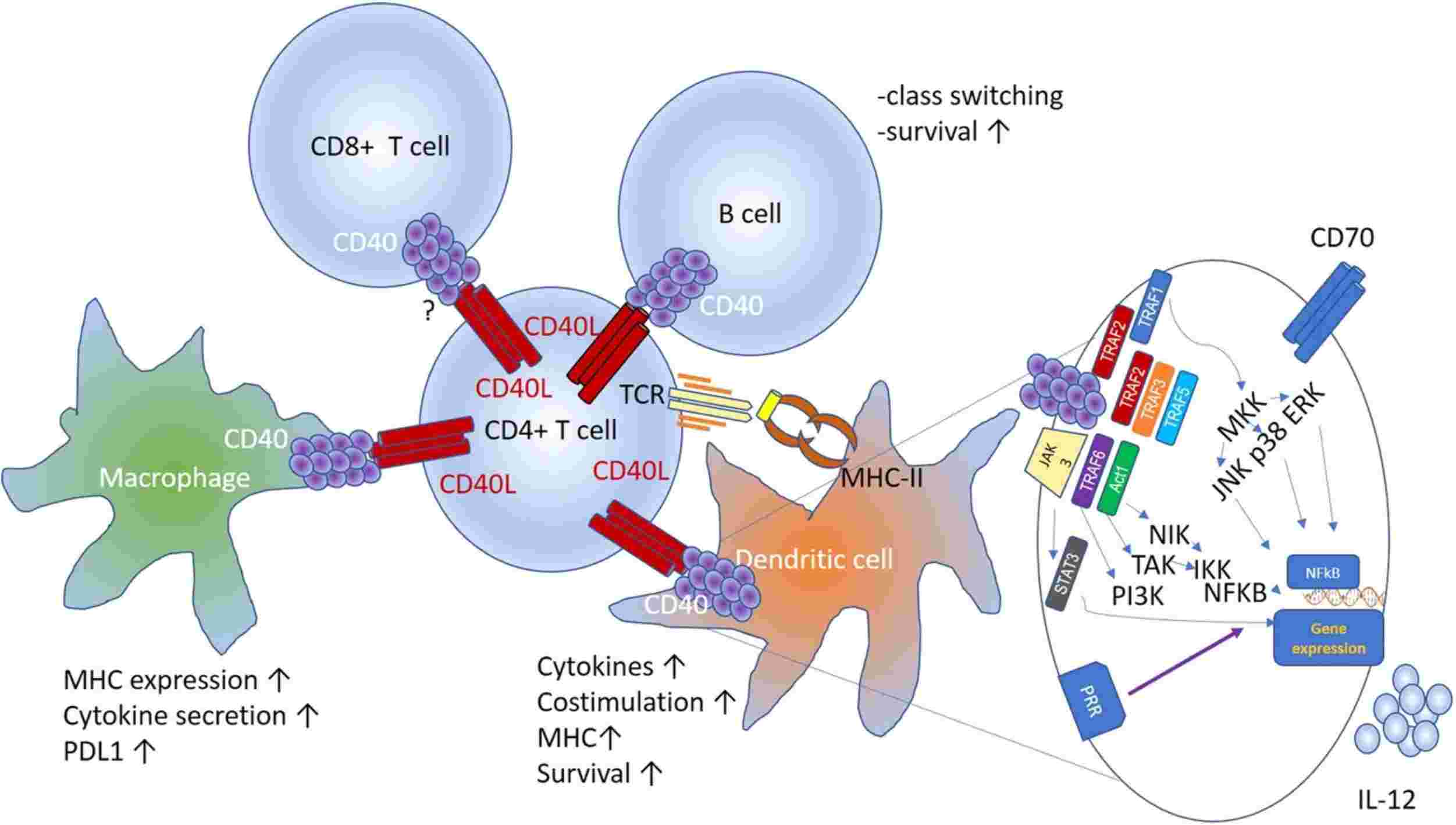
Figure 1. Schematic of the interactions between CD40L expressed by activated CD4+ T cells and other cellular components of the tumor microenvironment. (Bullock T N J, et al., 2022)
CD40 Related Signaling Pathway
The signaling pathway mediated by CD40 is intricate and tightly regulated. Upon ligand binding, CD40 activates various signaling pathways, including the canonical NF-κB pathway and the MAPK pathway. These pathways culminate in the modulation of gene expression, orchestrating immune responses, and shaping the fate of immune cells.
Activation of NF-κB induces the expression of pro-inflammatory cytokines and anti-apoptotic proteins, promoting cell survival and immune activation. Simultaneously, the MAPK pathway contributes to cellular proliferation and differentiation, further amplifying the immune response. The precise orchestration of these pathways is essential for the finely tuned regulation of immune reactions.
CD40 Related Diseases
Dysregulation of CD40 signaling has been implicated in various diseases, highlighting the importance of this protein in maintaining immune homeostasis. In autoimmune disorders, aberrant CD40 activation can contribute to excessive inflammation and tissue damage. Additionally, CD40 has been implicated in the pathogenesis of certain cancers, as its overexpression can fuel uncontrolled cell proliferation and survival.
Moreover, deficiencies or mutations in CD40 or CD40L genes have been associated with immunodeficiency disorders, such as Hyper-IgM syndrome. Understanding the role of CD40 in these diseases provides valuable insights into potential therapeutic interventions.
CD40's Applications in Biomedicine
The multifaceted nature of CD40 has paved the way for its applications in biomedical research and development. In diagnostics, the detection of CD40 expression levels can serve as a biomarker for certain diseases, aiding in early diagnosis and prognosis. This has implications for personalized medicine and targeted therapies.
In vaccine development, harnessing the CD40-CD40L interaction has proven instrumental. Targeting CD40 on antigen-presenting cells can enhance the efficacy of vaccines, eliciting robust immune responses. This approach is particularly promising in the development of vaccines against infectious diseases and cancer.
Furthermore, therapeutically, modulating CD40 signaling is a burgeoning area of research. Agonists and antagonists targeting CD40 are being explored as potential immunomodulatory agents. These agents hold promise in the treatment of autoimmune disorders, cancer, and immunodeficiencies, offering a new frontier in precision medicine.
Recommended Products
Reference
- Bullock T N J. CD40 stimulation as a molecular adjuvant for cancer vaccines and other immunotherapies. Cellular & molecular immunology. 2022, 19(1): 14-22.

