Smooth Muscle Cell Markers
Related Symbol Search List
Immunology Background
Overview of Smooth Muscle Cell Markers
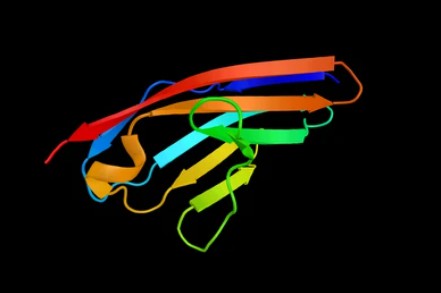
Under specific conditions, mesenchymal stem cells (MSCs) can differentiate into unique cell types, making them attractive candidates for cell-based disease therapies, such as the ability of MSCs to differentiate into smooth muscle cells (SMCs). Smooth muscle cell markers are specific molecules or proteins used to identify and localize smooth muscle cells. They are widely used in research, not only to help us understand and characterize smooth muscle cells but also as key factors in the directed differentiation of mesenchymal stem cells (MSCs) into smooth muscle cells. Commonly used markers include α-smooth muscle actin (α-SMA), smooth muscle myosin heavy chain (SM-MHC), calponin, and smoothelin. Using these markers, researchers can track the differentiation of MSCs to smooth muscle cells and study the mechanisms involved. By using immunohistochemistry or molecular techniques, researchers can quantify or localize these markers to achieve accurate detection of smooth muscle cells and their differentiation status.
Research Areas of Smooth Muscle Cell Markers
There is a wide range of areas in which people are researching the application of smooth muscle cell markers as differentiation factors for MSCs. Some of the detailed areas of research are given below:
- Cardiovascular disease research
The use of smooth muscle cell markers in MSC differentiation can facilitate cardiovascular disease research. By using these markers, researchers can direct the differentiation of MSCs into smooth muscle cells and further construct vascular tissues with functionality, thus providing the basis for vascular regeneration and cardiovascular disease treatment. Some studies have indicated (Gu W, et al., 2017) that differentiation of MSCs into vascular cells can directly participate in the formation of new blood vessels to restore blood flow and can enhance the regeneration of existing blood vessels in vivo through secreted trophic factors. However, more evidence is still needed to determine the direct contribution of smooth muscle cells and endothelial cells differentiated from MSCs in vivo.
- Bioengineered blood vessels
Bioengineered blood vessels consist of three key components, which are cells, biodegradable scaffolds, and humoral or mechanical signals. Growing a layer of endothelial cells within a scaffold has been shown to improve the antithrombotic and clinical outcomes of vascular grafts. And implantation of smooth myocytes on biodegradable scaffolds can enhance arterial wall regeneration. However, the limited lifespan of mature endothelial cells and smooth muscle cells and the need for long culture time limit their application in tissue engineering. MSCs are a valuable source of cells that can overcome these limitations due to their multispectral differentiation potential. Bone marrow-derived MSCs are one of the most widely studied MSC types. By transforming bone marrow MSCs into small-diameter blood vessels, significant similarity to natural blood vessels can be achieved at the histologic and molecular levels (Zhang L, et al., 2008. Hjortnaes J, et al., 2010. Zhang J, et al., 2006).
- Tissue engineering research
Like bioengineered blood vessels, researchers can build tissue-engineered structures with biomechanical properties by directing the differentiation of MSCs into smooth muscle cells. These structures can be used to mimic the function of real tissues, such as artificial blood vessels, artificial esophagus, and artificial implants, and are important in biomedical research and therapy (Jung Y, et al., 2015).
- In vitro model for drug screening and toxicity testing
With smooth muscle cell markers as MSC differentiation factors, researchers can construct more accurate and physiologically relevant in vitro models for drug screening and toxicity testing. By differentiating MSCs into smooth muscle cells, these in vitro models can be used to assess the efficacy and safety of specific drugs, helping to increase the efficiency of new drug development and reduce the need for animal testing.
Overall, smooth muscle cell markers have a wide range of applications as MSC differentiation factors in the fields of cardiovascular disease, tissue engineering, drug screening, and toxicity testing. These studies can help promote the development of regenerative medicine and provide more individualized and customized treatments for clinical applications.
Reference:
- Gu W, Hong X, Potter C, Qu A, Xu Q. Mesenchymal stem cells and vascular regeneration. Microcirculation. 2017 Jan;24(1). doi: 10.1111/micc.12324. PMID: 27681821.
- Zhang L, Zhou J, Lu Q, Wei Y, Hu S. A novel small-diameter vascular graft: In vivo behavior of biodegradable three-layered tubular scaffolds. Biotechnol Bioeng. 2008; 99: 1007–1015.
- Hjortnaes J, Gottlieb D, Figueiredo JL et al. Intravital molecular imaging of small-diameter tissue-engineered vascular grafts in mice: a feasibility study. Tissue Eng Part C Methods. 2010; 16: 597–607.
- Zhang J, Qi H, Wang H, et al. Engineering of vascular grafts with genetically modified bone marrow mesenchymal stem cells on poly (propylene carbonate) graft. Artif Organs. 2006; 30: 898–905.
- Jung Y, Ji H Y, Chen Z, et al. Scaffold-free, human mesenchymal stem cell-based tissue-engineered blood vessels [J]. Scientific Reports, 2015, 5(1): 15116.

