T Cell Markers
Related Symbol Search List
Immunology Background
Background
T cell markers are specific molecules expressed on the surface of T cells or found within T cells that serve as identifiers or indicators of T cell subsets, activation status, and functional properties. These markers play a crucial role in characterizing and classifying T cells and are widely used in immunology research and clinical diagnostics. By examining the expression of different T cell markers, researchers and clinicians can gain insights into T cell populations, immune responses, and disease states. Here is an introduction to some commonly used T cell markers:
Cluster of Differentiation (CD) Markers
CD markers are cell surface molecules identified by monoclonal antibodies targeting specific proteins. CD molecules are numbered sequentially and are widely used to classify and distinguish different cell types, including T cells. Examples include CD3, CD4, CD8, and CD25.
Transcription Factors
Transcription factors are proteins that regulate gene expression and control the differentiation and function of T cell subsets. Specific transcription factors are associated with different T cell lineages. Examples include T-bet (T-box expressed in T cells), ATA-3, RORγt (RAR-associated orphan receptor gamma), Foxp3 (forkhead box P3).
Activation and Proliferation Markers
Various markers indicate the activation and proliferation status of T cells. These markers are upregulated upon T cell activation and can provide insights into the immune response. Examples include CD69, CD25, Ki-67.
Chemokine Receptors
Chemokine receptors are involved in T cell migration and homing to specific tissues or inflammatory sites. They play a crucial role in directing T cell responses. Examples include CCR7, CXCR3, CCR4 and CCR8.
These are just a few examples of the many T cell markers used in immunology research and diagnostics. The expression patterns of these markers can provide valuable information about T cell subsets, activation status, functional properties, and their involvement in immune responses and diseases. By studying these markers, researchers aim to better understand T cell biology, develop targeted therapies, and monitor immune-related disorders.
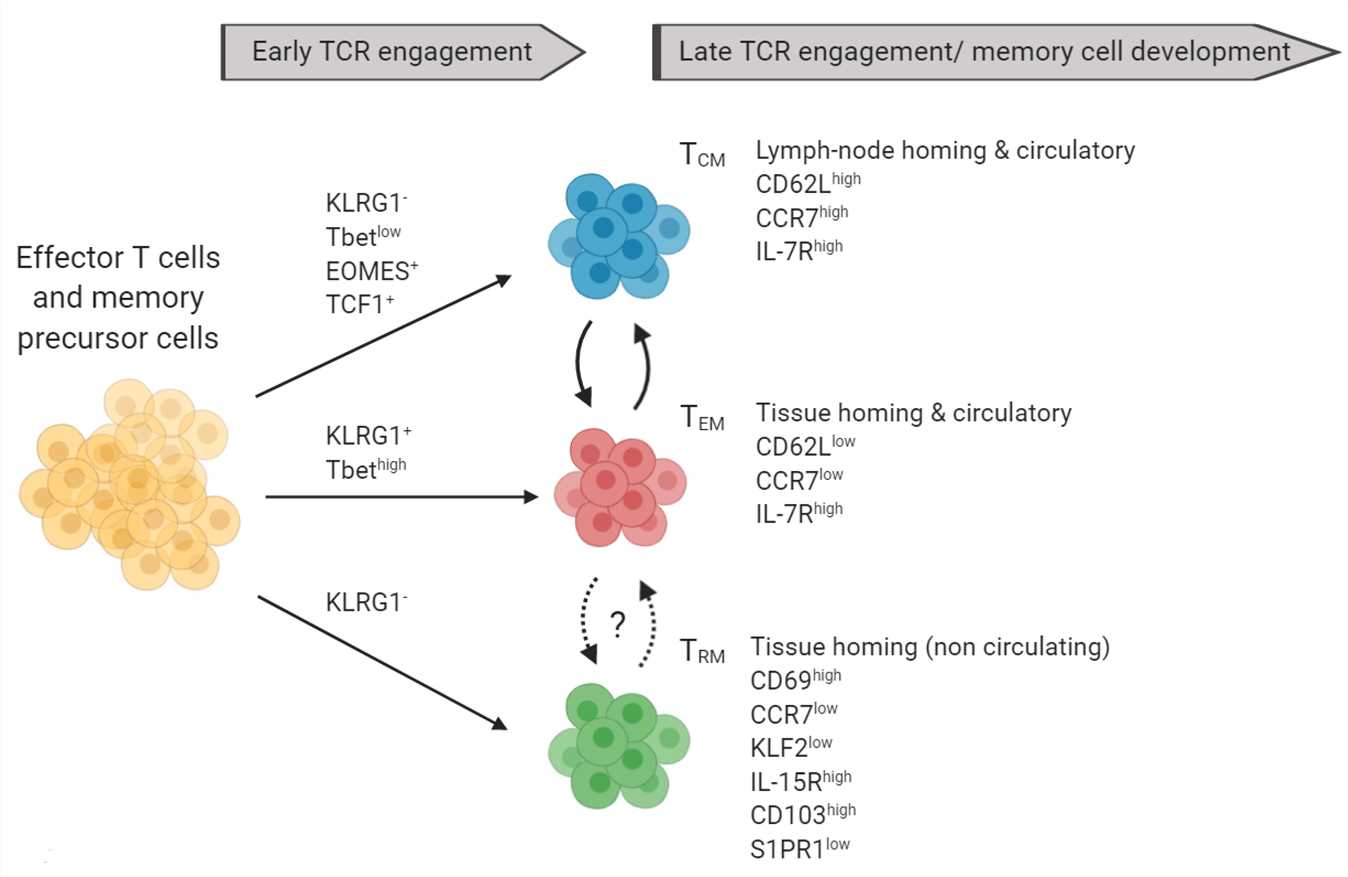 Fig.1 Markers of memory T cell subsets and their precursors: Terminally differentiated TCM (blue) and TEM (red) can be distinguished based on the expression of CD62L, CCR7, IL7R, and other markers not shown. (Raphael I, et al., 2020)
Fig.1 Markers of memory T cell subsets and their precursors: Terminally differentiated TCM (blue) and TEM (red) can be distinguished based on the expression of CD62L, CCR7, IL7R, and other markers not shown. (Raphael I, et al., 2020)Types of T Cell Markers
T cell markers can be categorized into three main types based on their location and function: surface markers, intracellular markers, and activation markers.
| Types | Functions |
|---|---|
| Surface Markers | Surface markers are proteins found on the cell membrane of T cells. They are commonly used to identify and classify different T cell subsets. Some examples of surface markers include:
|
| Intracellular Markers | Intracellular markers are proteins found within the cytoplasm or nucleus of T cells. They are often used to identify specific T cell subsets and functional properties. Some examples of intracellular markers include:
|
| Activation Markers | Activation markers are proteins that are upregulated upon T cell activation. They are used to assess T cell activation status and response to stimuli. Some examples of activation markers include:
|
These different types of T cell markers provide valuable information about T cell subsets, activation status, and functional properties. By analyzing the expression of these markers, researchers and clinicians can gain insights into immune responses, disease states, and the efficacy of immune interventions.
Role of T Cell Markers in Diseases
T cell markers play a crucial role in understanding and diagnosing various diseases. The expression patterns of T cell markers can provide insights into the immune response, disease progression, and treatment strategies. Here are some examples of how T cell markers are involved in different diseases:
Autoimmune Diseases
Autoimmune diseases occur when the immune system mistakenly attacks the body's own tissues. T cell markers are often used to assess T cell involvement in these diseases. For example:
- In multiple sclerosis (MS), the presence of CD4+ T cells and CD8+ T cells in the central nervous system indicates their role in the immune response targeting myelin.
- In rheumatoid arthritis (RA), the presence of activated T cells expressing markers such as CD25 and CD69 in the joint tissue contributes to inflammation and tissue damage.
Infectious Diseases
T cell markers are important in understanding the immune response to infectious agents. Monitoring T cell markers helps determine the effectiveness of the immune response and can aid in diagnosing and managing infections. For instance:
- In HIV/AIDS, a decline in CD4+ T cell count is a hallmark of disease progression, leading to immune dysfunction and increased susceptibility to opportunistic infections.
- In tuberculosis (TB), the presence of T cells expressing markers such as interferon-gamma (IFN-γ) and tumor necrosis factor-alpha (TNF-α) indicates an active immune response against the Mycobacterium tuberculosis bacterium.
Cancer
T cell markers are crucial in cancer immunology and immunotherapy. They help identify tumor-infiltrating lymphocytes and assess the immune response against cancer cells. Examples include:
- In melanoma, the presence of tumor-infiltrating CD8+ T cells is associated with a favorable prognosis and response to immunotherapy.
- In hematological malignancies like lymphoma, the expression of specific T cell markers can aid in subclassification and determining treatment options.
Transplant Rejection
T cell markers are used to assess T cell-mediated rejection in organ transplantation. Monitoring markers such as CD3, CD4, and CD8 can help determine the presence and activity of T cells targeting the transplanted organ.
Immunodeficiencies
T cell markers are involved in diagnosing and monitoring immunodeficiency disorders. For example:
- Severe combined immunodeficiency (SCID) is characterized by impaired T cell development and reduced expression of CD3, CD4, and CD8 markers.
- DiGeorge syndrome, characterized by thymic hypoplasia, presents with reduced T cell populations and abnormalities in markers such as CD3 and CD4.
These are just a few examples of how T cell markers contribute to understanding diseases. By studying the expression and functions of T cell markers, researchers and clinicians can gain insights into disease mechanisms, develop diagnostic tools, and design targeted therapies to modulate T cell responses for improved patient outcomes.
Case Study
Case 1: Antoine Goury, et al. Deletion of receptor for advanced glycation end products exacerbates lymphoproliferative syndrome and lupus nephritis in B6-MRL Fas lpr/j mice. The Journal of Immunology 194.8 (2015): 3612-3622.
We generated mice invalidated for RAGE in the lupus-prone B6-MRL Fas lpr/j background to determine the role of RAGE in the pathogenesis of systemic lupus erythematosus. We compared the phenotype of these mice with that of their wild-type and B6-MRL Fas lpr/j littermates.
Lymphoproliferative syndrome, production of anti-dsDNA Abs, lupus nephritis, and accumulation of CD3+B220+CD4−CD8− autoreactive T cells (in the peripheral blood and the spleen) were significantly increased in B6-MRL Fas lpr/j RAGE−/− mice compared with B6-MRL Fas lpr/j mice.
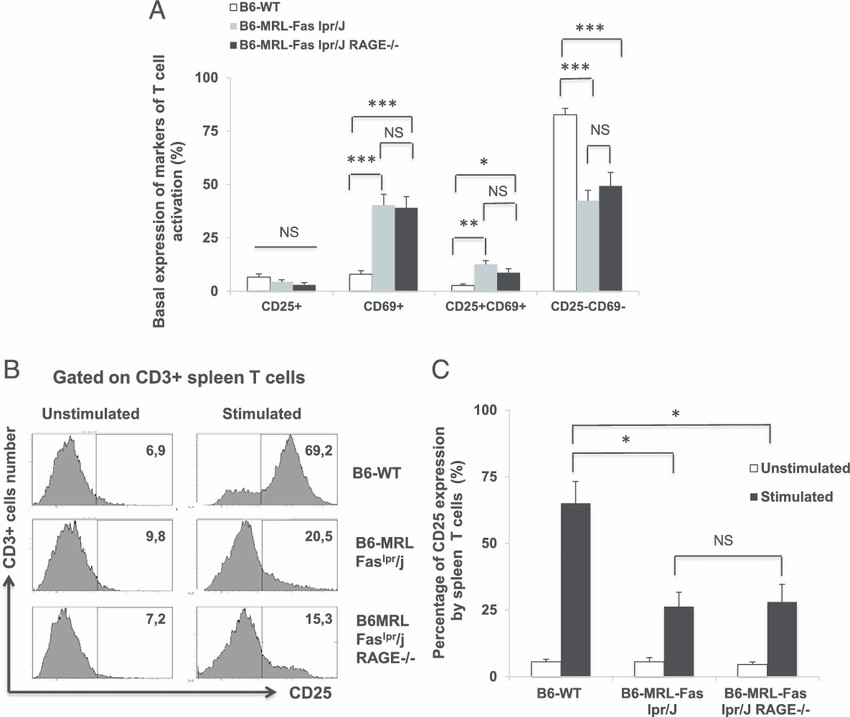 Fig.1 Analysis of T cell activation markers.
Fig.1 Analysis of T cell activation markers.Case 2: Lilian Lacerda Bueno, et al. Plasmodium vivax: induction of CD4+ CD25+ FoxP3+ regulatory T cells during infection are directly associated with level of circulating parasites. PLoS One 5.3 (2010): e9623.
Circulation CD4+CD25+FoxP3+ regulatory T cells (Tregs) have been associated with the delicate balancing between control of overwhelming acute malaria infection and prevention of immune pathology due to disproportionate inflammatory responses to erythrocytic stage of the parasite. Once observed the elevated number of Treg cells in the peripheral blood of infected donors, we further characterized this cell population by evaluating the expression of molecules and cytokines associated with cell modulation. Surface expression of the GITR molecule and intracellular expression of CTLA-4 and cytokines were evaluated by flow cytometry. P. vivax-infected individuals presented a significant increase of circulating GITR+ (A) and CTLA-4+ Treg cells (B), when compared to malaria-naïve donors.
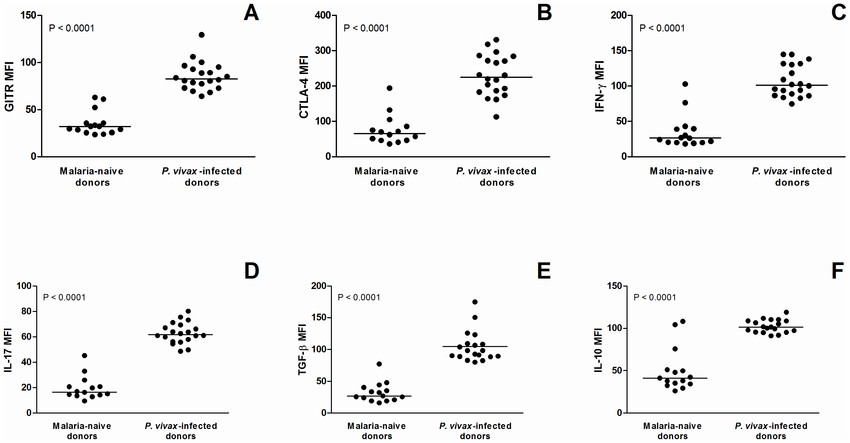 Fig.2 Expression of surface markers (CTLA-4 and GITR) and cytokines (IFN-γ, IL-17, TGF-β, and IL-10) on CD4+CD25+FoxP3+ regulatory T cells in malaria-naïve and P. vivax-infected donors.
Fig.2 Expression of surface markers (CTLA-4 and GITR) and cytokines (IFN-γ, IL-17, TGF-β, and IL-10) on CD4+CD25+FoxP3+ regulatory T cells in malaria-naïve and P. vivax-infected donors.References
- Williams-Gray C H, et al. Abnormalities of age-related T cell senescence in Parkinson’s disease. Journal of Neuroinflammation 15 (2018): 1-8.
- Antoine Goury, et al. Deletion of receptor for advanced glycation end products exacerbates lymphoproliferative syndrome and lupus nephritis in B6-MRL Fas lpr/j mice. The Journal of Immunology 194.8 (2015): 3612-3622.
- Raphael I, Joern RR, Forsthuber TG. Memory CD4+ T Cells in Immunity and Autoimmune Diseases. Cells. 2020; 9(3):531.

