MNP for Cell Therapy Research - Accelerating Next-Generation CAR-T Cell Development
A New Paradigm for CAR-T Target Validation
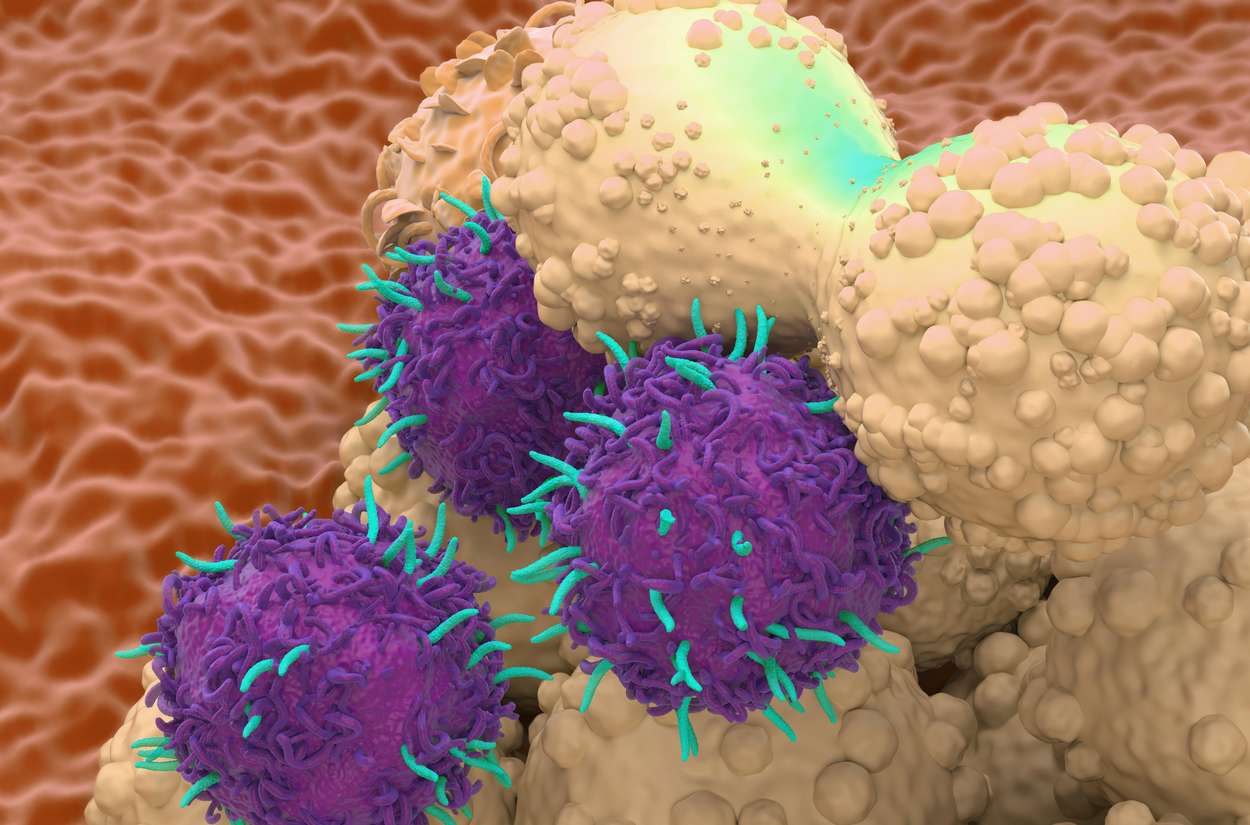
The clinical success of CAR-T cell therapies has revolutionized cancer treatment, yet significant challenges persist in preclinical development. Traditional target validation relies heavily on engineered cell lines or primary tumor cells, which often present inconsistent antigen expression, batch-to-batch variability, and biosafety concerns. Membrane Protein Nanoparticles (MNPs)—nanoparticles coated with natural cell membranes embedded with native membrane proteins—are emerging as a transformative platform that recapitulates physiological antigen presentation with unprecedented precision and control.
This technology fundamentally changes how researchers approach CAR-T development by providing a modular, standardized, and physiologically relevant tool for every stage of the pipeline, from early scFv screening to clinical CMC quality control.
Explore MNPs Products
Learn More
Advantages of MNP-Based Tumor Antigen Presentation
MNPs replicate the native tumor cell surface architecture with several distinct advantages over conventional systems:
Native Conformational Integrity: Unlike recombinant protein fragments or synthetic peptides, MNPs preserve full-length transmembrane proteins in their natural lipid bilayer environment. This maintains critical post-translational modifications (glycosylation, palmitoylation), proper quaternary structure, and authentic orientation—essential for conformational epitopes that many CAR-T therapies target.
Quantitative Control: Researchers can precisely tune antigen density on MNP surfaces through controlled protein insertion during manufacturing, enabling systematic studies of antigen density thresholds—a parameter impossible to control with tumor cell lines that exhibit heterogeneous expression.
Scalability and Standardization: MNP production yields homogeneous, stable reagents that eliminate batch-to-batch variability plaguing primary cell cultures. Lyophilized MNPs maintain activity for 12+ months at 4°C, enabling multi-site clinical studies and commercial manufacturing with consistent positive controls.
Safety and Accessibility: MNPs eliminate the need for handling live tumor cells or radioactive materials in functional assays, reducing biosafety level requirements and enabling high-throughput screening in standard BSL-2 laboratories.
Solving the Transmembrane Protein Expression Challenge
A critical bottleneck in CAR-T development involves validating targets that are difficult to express in traditional heterologous systems. Complex multi-pass transmembrane proteins like CLDN6 (a tight junction protein and promising solid tumor target) often misfold or aggregate when expressed in 293T or CHO cells, yielding non-physiological epitopes.
The MNP Solution: By sourcing membranes from cells that natively express the target protein (e.g., CLDN6-positive ovarian cancer cells) or using viral-like particle (VLP) insertion systems, MNPs circumvent expression challenges entirely. The protein is harvested in its native state, then reconstituted onto nanoparticle surfaces at defined densities.
Case Example—GPC3 for Hepatocellular Carcinoma: Glypican-3, a GPI-anchored protein, loses critical glycosylation patterns when expressed in non-hepatic cell lines. MNPs generated from HCC cell membranes retain tumor-specific glycoforms, enabling development of CAR-T cells that recognize authentic clinical epitopes, improving translational relevance.
This approach similarly benefits validated blood cancer targets like CD20, where subtle conformational differences between recombinant protein and native B-cell membrane presentation can impact CAR-T binding kinetics and clinical performance.
scFv Affinity and Specificity Evaluation Workflow
FACS Binding Assay: Optimized Incubation Conditions
MNP-based flow cytometry binding assays provide quantitative assessment of CAR-T scFv affinity under physiological conditions:
Protocol Parameters:
- MNP Concentration: 1-50 µg/mL total membrane protein, titrated based on target antigen density
- Cell Number: 2×10⁵ CAR-T cells per reaction
- Incubation Buffer: PBS + 2% FBS + 0.5 mM Ca²⁺/Mg²⁺ (maintains membrane integrity)
- Temperature: 4°C for equilibrium binding (prevents internalization) or 37°C for kinetic studies
- Time: 30-60 minutes with gentle agitation
- Detection: Fluorescently labeled anti-Fab secondary antibody or protein L
Critical Optimization: Include 10% human AB serum to block Fc receptors and reduce non-specific binding. For CARs with murine scFv frameworks, add anti-murine IgG Fc blocking antibody.
Titration Curves and EC50 Determination
Generate dose-response curves by serially diluting MNPs (1:3 dilutions across 10-12 concentrations) while maintaining constant CAR-T cell numbers. Plot median fluorescence intensity (MFI) versus MNP concentration and fit with a four-parameter logistic model:
EC50 Calculation: The half-maximal effective concentration reflects apparent binding affinity. For lead optimization, aim for EC50 values between 10-100 ng/mL for optimal therapeutic window—affinities tighter than 1 ng/mL risk on-target/off-tumor toxicity, while values >500 ng/mL may indicate insufficient potency.
Quality Metrics: Include Hill slope analysis (should be 1.0±0.3 for monovalent binding) and R²>0.95. Run each titration in triplicate across three independent MNP batches to assess reproducibility.
Cross-Reactivity Panel: Rapid Off-Target Risk Assessment
The MNP array platform enables simultaneous screening against 50+ off-target tissues in a single experiment:
Panel Design: Create MNPs from membrane preparations of:
- Human heart, liver, kidney, lung (major organs)
- Primary epidermal keratinocytes, colon epithelium (toxicity concerns)
- Tissue-specific stem cells (risk of irreversible damage)
- Related family members (e.g., HER2 when targeting HER3)
Execution: Multiplex with distinct fluorescence codes (e.g., MNPs labeled with different APC/Cy7 ratios) and incubate with CAR-T cells at 10×EC50 concentration to maximize detection of low-affinity cross-reactivity.
Data Analysis: Calculate cross-reactivity index (CRI = MFI_target / MFI_off-target). A CRI >100-fold is generally acceptable; 10-100-fold requires tissue-specific expression analysis; <10-fold indicates high off-target risk requiring scFv engineering.
This comprehensive screen condenses 6 months of traditional in vivo toxicity studies into 48 hours of in vitro analysis, accelerating lead candidate selection while reducing animal use.
Functional Experimental Design
Cytokine Release Assay: Quantifying CAR-T Activation
MNPs serve as potent, controllable stimulators for measuring effector function:
Experimental Setup:
- Plate CAR-T cells at 1×10⁵ cells/well in 96-well round-bottom plates
- Add MNPs at varying antigen densities (10² to 10⁵ molecules per MNP)
- Co-culture for 24 hours at 37°C, 5% CO₂
- Harvest supernatants for multiplex cytokine analysis
Key Readouts:
- IFN-γ: Primary activation marker; ED50 (effective dose for 50% max response) should correlate with EC50
- IL-2: Indicates proliferative capacity; IL-2/IFN-γ ratio predicts in vivo persistence
- TNF-α: High levels may predict cytokine release syndrome risk
- GM-CSF: Correlate with neurotoxicity potential
Advanced Application: Use time-course sampling (4, 8, 12, 24h) to construct activation kinetics profiles. Early IL-2 peak suggests rapid activation; delayed IFN-γ may indicate exhaustion-prone CAR-T phenotypes.

Cytotoxicity Assay: MNP-Coated Target Cells
Traditional chromium-51 release assays are being replaced by MNP-based systems:
Methodology:
- Coat magnetic or fluorescent nanoparticles with tumor cell membranes containing target antigen
- Label with cell viability dye
- Incubate with CAR-T cells at E:T ratios from 10:1 to 0.1:1
- After 4-16 hours, quantify surviving targets via flow cytometry or fluorescence microscopy
Explore Fluorescent Dyes
Learn More
Innovation: The "MNP killing" assay enables real-time imaging of immune synapse formation using nanoparticles with pH-sensitive dyes that fluoresce upon acidification in the immunological synapse, directly visualizing CAR-T engagement quality.
Specific Lysis Calculation: % Specific Lysis = (1 - (Target_CAR-T / Target_no_effector)) × 100
Antigen Density Threshold Studies
A breakthrough application uses density-tuned MNPs to define minimal antigen density required for CAR-T activation:
Density Calibration: Create MNPs with precisely controlled antigen molecules per particle:
- Low: 10²-10³ (mimics low-expressing normal tissues)
- Medium: 10³-10⁴ (typical tumor expression)
- High: 10⁴-10⁵ (over-expressing tumors)
Threshold Determination: The minimum antigen density that elicits >20% of maximal cytokine release defines the activation threshold. For clinical safety, ensure this threshold is ≥10-fold higher than expression on vital normal tissues.
Clinical Translation: This data directly informs patient selection criteria—only patients whose tumors exceed the defined antigen density threshold should be enrolled, maximizing therapeutic index.
Clinical Translation and CMC Integration
Monitoring Patient-Derived CAR-T Expansion
Autologous CAR-T manufacturing requires robust quality control throughout the 7-14 day expansion period:
Day 3 Functional Check: Expose early-stage CAR-T cultures to MNPs bearing target antigen. Poor IFN-γ response (<200 pg/mL) predicts manufacturing failure, enabling early process intervention (e.g., IL-7/IL-15 supplementation).
Final Product Potency: FDA guidance requires potency assays for release. MNP-stimulated cytokine production provides a standardized, donor-independent potency metric that correlates with clinical response. Establish product release specifications: e.g., IFN-γ >1000 pg/mL when stimulated with 10⁴ antigen molecules/MNP.
CMC Quality Control Positive Controls
MNPs serve as ideal reference standards in chemistry, manufacturing, and controls (CMC):
Lot Release Assay Validation: Use MNPs as consistent positive controls for:
- Flow cytometry CAR detection (CD3/CD4/CD8/CAR co-staining)
- Cytotoxicity assay validation
- Cytokine release assay standardization
Stability Studies: MNPs lyophilized with trehalose maintain consistent EC50 values for 18 months at 25°C, enabling deployment as global reference standards without cold chain dependency.
Regulatory Filing Support: Include MNP-based characterization data in IND applications to demonstrate:
- Specificity (cross-reactivity panel results)
- Potency (EC50 and ED50 values)
- Durability (antigen density threshold data)
Target-Specific Development Roadmaps
CLDN6 CAR-T for Solid Tumors
Challenge: CLDN6 is a four-pass transmembrane tight junction protein with no extracellular cysteines for labeling, making recombinant production impossible.
MNP-Based Roadmap:
- Target Validation: Generate MNPs from CLDN6-positive PA-1 teratocarcinoma cells; confirm absence in CLDN6-negative tissues via cross-reactivity panel
- scFv Discovery: Screen phage libraries using CLDN6-MNPs for conformational epitope binders; isolate 5-10 unique clones
- Lead Optimization: Characterize affinity (EC50 15-45 ng/mL range) and specificity (CRI >500-fold vs. CLDN3/4 family members)
- Potency Metrics: Demonstrate robust IFN-γ release at antigen densities as low as 500 molecules/MNP
- Clinical QC: Deploy CLDN6-MNPs as lot release potency standard
CD20 CAR-T for Hematological Malignancies
Challenge: CD20 density varies 100-fold across B-cell malignancies and normal B-cells; optimizing therapeutic window is critical.
MNP-Based Roadmap:
- Density Modeling: Create CD20-MNP series mimicking:
- Normal B-cells: 10³ molecules/MNP
- Low-grade lymphoma: 5×10³ molecules/MNP
- High-grade lymphoma: 2×10⁴ molecules/MNP
- Affinity Tuning: Engineer scFv variants with EC50 values of 25-75 ng/mL to spare normal B-cells while killing tumor cells
- Combination Studies: Use MNPs co-expressing CD20+CD22 to evaluate dual CAR strategies; demonstrate synergistic killing at sub-threshold densities
- Biosimilar Development: For CD20 biosimilar CAR-T products, MNPs provide reference standard for comparative binding assays per FDA biosimilar guidance
Implementation Guidelines and Best Practices
MNP Selection Criteria:
- Particle size: 50-200 nm optimal for cellular uptake and FACS detection
- Membrane source: Align with target's native tissue for proper PTMs
- Quality metrics: >90% target protein incorporation efficiency, <5% aggregation
Explore MNPs Products
Learn More
Assay Validation:
- Demonstrate parallelism between MNP and authentic tumor cell results before adopting MNP-only workflows
- Establish qualified antigen density measurement using quantitative mass spectrometry
- Implement bridge studies comparing historical tumor cell data with MNP data for regulatory continuity
Troubleshooting:
- High background: Increase washing stringency (0.05% Tween-20) or add 2% BSA blocking step
- Low signal: Verify CAR surface expression; try biotinylated MNPs with streptavidin-fluorochrome amplification
- Batch variation: Implement MNP master stocks with full characterization; aliquot and store at -80°C
Conclusion
Membrane Protein Nanoparticles are not merely research tools—they represent a paradigm shift in CAR-T cell therapy development. By providing native, controllable, and scalable antigen presentation, MNPs streamline target validation, accelerate lead optimization, and provide robust CMC solutions that meet regulatory expectations. As the field advances toward solid tumors and complex antigens, MNP technology will become indispensable for developing the next generation of safer, more effective cell therapies. Integration of MNP workflows from discovery through clinical manufacturing ensures data continuity, reduces development timelines by 40-60%, and ultimately delivers more predictable clinical outcomes for patients awaiting these life-saving therapies.
Ready to accelerate your CAR-T program? Contact our team to access our catalog of pre-validated MNPs or discuss custom development for your proprietary targets.
Related Products and Services
Resource
-
Unlocking Drug Targets with Membrane Protein Nanoparticles!
-
Membrane Protein Platforms: 6-Way Showdown!
-
Mastering Membrane Protein Platforms in 3 Minutes!
Contact us or send an email at for project quotations and more detailed information.
Quick Links
-

Papers’ PMID to Obtain Coupon
Submit Now -

Refer Friends & New Lab Start-up Promotions

