Inflammatory Bowel Diseases Therapeutic Targets
Related Symbol Search List
Immunology Background
Available Resources for Study of Inflammatory Bowel Diseases Therapeutic Targets
Creative BioMart is committed to being at the forefront of IBD research. Our priority is to ensure that researchers have access to the latest tools and information to drive progress in this important field of study.
- We offer a wide range of products, including recombinant proteins and other essential materials that play a crucial role in uncovering the mechanisms of IBD. We understand that each researcher has unique requirements, which is why we provide a diverse selection of products tailored to their specific needs.
- Our team of experienced experts in IBD research are incredibly knowledgeable and dedicated to their work. They are committed to providing customized and individualized solutions to meet the specific requirements of every researcher.
- In addition, we offer comprehensive support resources that cover involved pathways, protein functions, interacting proteins, and other valuable information. Our goal is to empower researchers to gain a comprehensive understanding of IBD and amplify the impact of their research.
Our Featured Products
- Active Recombinant Human ICOS, Fc-His tagged
- Recombinant Human ICOS protein, Fc-tagged
- Recombinant Rat Icos, Fc tagged
- Recombinant Rat Icos Protein, Fc-tagged, FITC conjugated
- Recombinant Human PPARG, GST-tagged
- Recombinant Mouse Pparg protein, His-tagge
- Active Recombinant Human IFNG
- Recombinant Human IL12A protein, Fc-tagged
- Recombinant Human IL12A, His tagged
- Recombinant Human Adenosine Kinase, His-tagged
- Recombinant Human ADORA1, GST-tagged
- Active Recombinant Human IL1R2 protein, His-tagged
- Recombinant Human IL1R2 protein, Fc-tagged
- Recombinant Human IRF3 protein, His/T7-tagged
- Recombinant Human PDE7A, GST-tagged
- Recombinant Human PDE7A protein, His-tagged
- Recombinant Human RELA Protien, GST-tagged
Whether you are studying IBD pathology, drug discovery or treatment development, Creative BioMart is here to support your research. We are committed to helping you achieve your scientific goals and make meaningful contributions to the field of IBD research. Contact us today to learn more about our products and resources.
About Inflammatory Bowel Diseases
Inflammatory Bowel Diseases (IBD) encompass a group of chronic inflammatory disorders that primarily affect the gastrointestinal tract. The two main types of IBD are Crohn's disease (CD) and ulcerative colitis (UC). These conditions are characterized by recurring inflammation in the digestive system, leading to various symptoms and potential complications.
The development of IBD involves a complex interplay of genetic, environmental, and immune factors. While the exact cause is not fully understood, the following mechanisms contribute to the pathogenesis of IBD:
Genetic Predisposition
- Genetic factors play a significant role in the development of IBD. Individuals with a family history of IBD have a higher risk of developing the condition.
- Multiple genes have been identified that contribute to the susceptibility of developing IBD. These genes are involved in regulating the immune response, inflammation, and the integrity of the gut barrier. Some of the genes implicated in the susceptibility to inflammatory bowel disease (IBD) include:NOD2/CARD15, IL23R, ATG16L1, IRGM, ECM1, HLA.
- NOD2/CARD15: This gene encodes a protein involved in recognizing bacterial components and activating an immune response. Mutations in NOD2/CARD15 have been associated with increased susceptibility to Crohn's disease.
- IL23R: Interleukin-23 receptor gene variants have been found to be protective against developing Crohn's disease and ulcerative colitis. IL23R plays a role in regulating the inflammatory response.
- ATG16L1: Autophagy-related 16-like 1 gene is involved in the autophagy process, which is important for eliminating intracellular pathogens and maintaining gut homeostasis. Mutations in this gene have been associated with an increased risk of developing Crohn's disease.
- IRGM: Immunity-related GTPase family M gene is another autophagy-related gene, and certain variants have been linked to an increased risk of Crohn's disease.
- ECM1: Extracellular matrix protein 1 gene encodes a protein vital in maintaining the integrity of the gut barrier. Variants in this gene have been associated with a higher susceptibility to ulcerative colitis.
- HLA genes: The human leukocyte antigen (HLA) complex plays a crucial role in immune regulation and recognizing foreign antigens. Variants in certain HLA genes, such as HLA-DRB1 and HLA-DQ2/DQ8, have been associated with an increased risk of developing IBD.
Dysregulated Immune Response
- IBD is considered an autoimmune condition, where the immune system mistakenly attacks the cells in the gastrointestinal tract.
- In individuals with IBD, the immune system overreacts to normal gut bacteria or other substances in the intestines, triggering an inflammatory response.
- Immune cells, including T cells, B cells, and various inflammatory mediators, become activated, leading to chronic inflammation in the gut.
Environmental Triggers
- Environmental factors are believed to play a role in the development and progression of IBD.
- Diet: Certain dietary factors, such as a high intake of processed foods, refined sugars, and saturated fats, may contribute to the development of IBD. However, the exact mechanisms are still being studied.
- Gut Microbiota: Alterations in the composition or function of the gut microbiota may disrupt the balance between the immune system and the microbes, leading to inflammation.
- Infections: Exposure to certain infections or changes in the gut microbial balance due to infections may trigger or exacerbate IBD symptoms.
Intestinal Barrier Dysfunction
- The intestinal barrier serves as a protective layer against harmful substances in the gut lumen, preventing them from crossing into the underlying tissue.
- In individuals with IBD, the intestinal barrier may become compromised, allowing bacteria and other luminal contents to interact with the immune system.
- Disruption of the epithelial barrier can lead to an exaggerated immune response and chronic inflammation.
Immune System Dysregulation
- Dysregulation of the immune system in individuals with IBD results in an abnormal immune response and chronic inflammation.
- Immune cells release pro-inflammatory cytokines and other mediators, leading to tissue damage and the characteristic symptoms of IBD.
The specific mechanisms and triggers may vary between individuals and between the two main types of IBD (Crohn's disease and ulcerative colitis). A better understanding of these mechanisms is crucial for developing targeted therapies and personalized treatment approaches for individuals with IBD.
Pathophysiology of Inflammatory Bowel Diseases
Antigen-presenting cells (APCs) and macrophages are activated and produce pro-inflammatory cytokines, including tumor necrosis factor (TNF), IL-6, IL-12, and IL-23. Activated APCs present processed antigens to naïve helper T cells (Tn) and promote the differentiation of Tn to effector T cells, helper T1 (Th1), Th2, and Th17 cells, and regulatory T (Treg) cells. Th1 and its innate counterpart innate lymphoid cells 1 (ILC1s) and natural killer (NK) cells release Th1 cytokines [interferon (IFN)-γ and TNF]; Th2 and ILC2 Th2 cytokines (IL-4, IL-5, and IL-13); Th17 and ILC3 Th17 cytokines (IL-17 and IL-22). Inflammation in lamina propria is involved in the migration and trafficking of lymphoid cells from blood vessels and lymph nodes where integrin and sphingosine-1-phosphase receptors (S1PR) are important. GSALT, gut-selective anti-lymphocyte trafficking. (Show as fig.1)
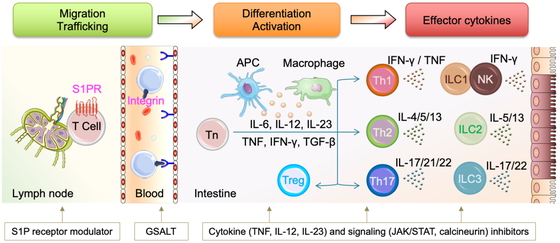 Fig.1 Pathophysiology of inflammatory bowel disease. (Mikami Y, et al., 2023)
Fig.1 Pathophysiology of inflammatory bowel disease. (Mikami Y, et al., 2023)
The Treatment Targets of Inflammatory Bowel Diseases
Therapeutic targets for Inflammatory Bowel Diseases (IBD) are actively being investigated to develop more effective treatment strategies. Several key targets have been identified, including cytokines, receptors, and signaling pathways. Here are some of the therapeutic targets and their related molecular mechanisms and pathogenic pathways analyzed in the context of IBD:
Tumor Necrosis Factor-alpha (TNF-α)
- TNF-α is a pro-inflammatory cytokine that plays a central role in the pathogenesis of IBD.
- Anti-TNF therapies, such as infliximab and adalimumab, have been successfully used to treat IBD by neutralizing TNF-α and reducing inflammation.
- Molecular mechanisms include blocking TNF-α binding to its receptors, inhibiting downstream signaling pathways, and reducing immune cell activation and migration.
Interleukin-12 (IL-12) and Interleukin-23 (IL-23)
- IL-12 and IL-23 are cytokines involved in the immune response and inflammation in IBD.
- Targeting IL-12 and IL-23 signaling pathways has shown promise in IBD treatment.
- Monoclonal antibodies like ustekinumab target the p40 subunit shared by IL-12 and IL-23, thereby inhibiting their effects on immune cells and reducing inflammation.
Integrins
- Integrins are cell adhesion molecules involved in immune cell trafficking and inflammation.
- Vedolizumab, an antibody targeting the α4β7 integrin, has been approved for IBD treatment.
- By blocking the interaction between immune cells and the gut tissue, vedolizumab helps reduce inflammation and control disease activity.
Janus Kinase (JAK) Inhibitors
- JAK inhibitors, such as tofacitinib and upadacitinib, target the JAK-STAT signaling pathway involved in immune cell activation and cytokine production.
- By inhibiting JAK enzymes, these drugs modulate the immune response and reduce inflammation in IBD.
Sphingosine-1-phosphate (S1P) Receptors
- S1P receptors are involved in immune cell migration and inflammation.
- S1P receptor modulators, such as ozanimod, target these receptors and regulate immune cell trafficking, thus reducing inflammation in IBD.
IL-6 Signaling Pathway
- IL-6 is a cytokine implicated in IBD pathogenesis. Targeting the IL-6 signaling pathway is being explored as a potential therapeutic approach.
- Monoclonal antibodies against the IL-6 receptor, such as tocilizumab, inhibit IL-6-mediated inflammation and have shown promise in IBD treatment.
Toll-like Receptors (TLRs)
- TLRs are pattern recognition receptors involved in the immune response to pathogens and the maintenance of gut homeostasis.
- Modulating TLR signaling is being investigated as a therapeutic target in IBD to regulate the immune response and limit inflammation.
MAPK Signaling Pathway
- The MAPK signaling pathway regulates various cellular processes, including inflammation.
- Inhibitors of MAPK pathway components are being studied as potential therapeutic targets to reduce inflammation in IBD.
Autophagy Pathway
- Autophagy is a cellular process involved in maintaining cellular homeostasis and regulating inflammation.
- Targeting autophagy-related proteins, such as ATG16L1 and NOD2, is being explored to modulate the inflammatory response in IBD.
These are just a few examples of therapeutic targets being investigated in IBD. The molecular mechanisms and pathogenic pathways associated with these targets provide insights into the underlying mechanisms of inflammation and suggest potential avenues for developing more targeted and personalized treatments for individuals with IBD.
Current and Future IBD Treatment Strategy
To further investigate potential targets for treating IBD, various molecules that contribute to the differentiation, induction, and activation of immune cells have been identified and many molecular targeted therapies against them have been applied clinically. Owing to high sample availability, most findings in human immunology have been obtained from immune cells in the peripheral blood and lymph nodes, and much remains unknown about the uniqueness of intestinal mucosal immunity. Because the intestinal tract is constantly exposed to foreign substances such as food and pathogens, mucosal immunity has a mechanism of maintaining intestinal homeostasis by forming a complex network of immune cells with the local environment of the intestinal tract, including intestinal bacteria and metabolites. Pursuing this local immune network in the intestinal local environment will enable us to elucidate the key chronic inflammatory mechanism of the intestinal tract.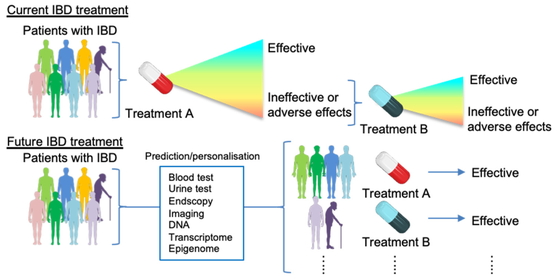 Fig.2 Current and future IBD treatment strategy. (Mikami Y, et al., 2023)
Fig.2 Current and future IBD treatment strategy. (Mikami Y, et al., 2023)
References:
- Mikami Y, Kanai T. Network Approaches to Uncover Pathogenesis and Therapeutic Targets of Inflammatory Bowel Diseases. Keio J Med. 2023;72(2):29-43. doi:10.2302/kjm.2022-0015-IR
- Agrawal M, Colombel JF. Treat-to-Target in Inflammatory Bowel Diseases, What Is the Target and How Do We Treat?. Gastrointest Endosc Clin N Am. 2019;29(3):421-436. doi:10.1016/j.giec.2019.02.004

